Dr Jenna Macciochi: There's evidence that endorphins are really helpful in how the immune system works. So if you're going on holiday and you find that you might have, if you have an autoimmune disease or an allergy or some kind of food intolerance, it might suddenly become a lot better when you go on holiday. And you just attribute that to eating a different kind of food, but it might be because you're happy when you're eating and that actually boosts these regulatory T cells that we have in our body that that sort of gently tap the brakes on the immune system and keep it in check.
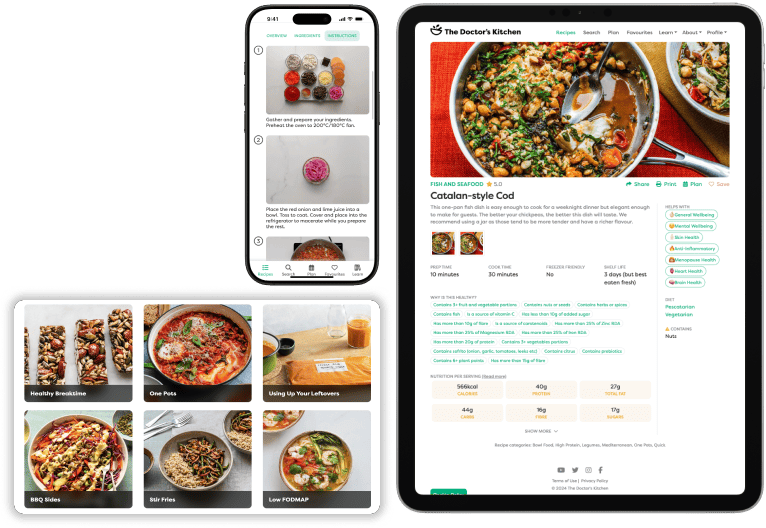
Dr Rupy: Welcome to the Doctor's Kitchen podcast. And in this series, we're going to be talking about the information that frames my next book, Eat to Beat Illness, that is out in March 2019. We're going to be continuing the sort of conversations that we started in my previous episodes of the Doctor's Kitchen podcast, like eating for brain health, skin function and mood. And we're going to be tackling lots more subjects in medicine where nutrition and lifestyle certainly have a role. In this series, we're going to be talking about how to practice lifestyle medicine alongside eating delicious food. Lifestyle medicine is primarily about getting to the root cause of medical problems rather than just symptom control. And our plates are a useful starting point for many of my patients. And as you'll find in this series, lots of doctors agree. Don't forget my first book, the bestselling Doctor's Kitchen is out now. So if you haven't got a copy, make sure you pick it up online or in all good book stores. Today, I'm inviting Dr Jenna Macciochi, I'm probably saying that wrong. Actually, it's Macciochi, which is an Italian surname, but she's actually hailing from Scotland to talk about eating for immunity. Now, Dr Jenna holds a PhD from the Faculty of Inflammation, Repair and Development at Imperial College, which is actually my old university. She's a lecturer in immunology at the University of Sussex who uses rigorous scientific research with the concepts old and new, holistic and conventional, to cultivate long-term health and well-being. Basically, a woman after my own heart. She's also editor at the scientific journal Annals of Advanced Biomedical Sciences, trained as a fitness instructor and a mother of twins. This is a fascinating two-part episode into immunity. What do we even mean by immunity? What does it encompass? What is the role of the immune system in the body beyond just fighting colds? And how do we support it if that is possible? I actually believe that the knowledge and the way we talk about immunity is misguided. And what I'm often asked is what can we do to boost or what supplements are there to increase my immune system activity, whereas actually that's probably not what we want to do. Topics include fasting therapies, autoimmune disease, the definition of plant hormesis, as well as the types of foods and lifestyle practices that are super important for immune health. You are going to absolutely love this episode. Let's kick off.
Dr Rupy: Jenna, welcome to the show.
Dr Jenna Macciochi: Thank you, Rupy. Thanks for having me.
Dr Rupy: This is, it's been a while since we've spoken, but we've finally got a date in the diary and yeah, so I'm really, really excited about this episode. I've been following your work for a little while as well. And the first time we met was at my book launch.
Dr Jenna Macciochi: Yes, yeah, yeah. We have a mutual friend and I came along. I already had your book at that point, actually.
Dr Rupy: Oh, did you? Oh, that's okay.
Dr Jenna Macciochi: So it was nice to come and see you celebrate that moment.
Dr Rupy: Yeah. It was a mutual friend of ours, John Payne, who's a photographer. And yeah, I remember him just saying, oh yeah, I brought my mate along. And then he told me you're an immunologist, you're interested in lifestyle medicine. I was like, that's amazing. That's great. And even back then, I was like, I think I must have said to you, we should get you on the podcast. That was back in January 2018.
Dr Jenna Macciochi: That was that long ago. Oh yeah, yeah.
Dr Rupy: We're here now.
Dr Jenna Macciochi: Finally made it.
Dr Rupy: So, we know a bit about you. We know that your background is in immunology. How did you get into this space where you're interested in diet and lifestyle? Do you have a personal story? Like, what's your background?
Dr Jenna Macciochi: Yeah, I mean, I grew up in rural Scotland. So, I grew up on a farm and I look back and I think, wow, that was a real privilege because it was very farm to table. And my mum was a professional cook. So she told me how everything she knew about cooking. But it was also an area of like a lot of rural poverty. There was a lot of industry closing, a lot of people that didn't have a lot. And I think that what growing up in that environment gave me was knowing how to cook and make something from nothing. And I think that's something that I think's been lost in today's society.
Dr Rupy: What whereabouts in rural Scotland was it?
Dr Jenna Macciochi: So it was in Ayrshire, on a farm. It was on the west coast.
Dr Rupy: Oh, I don't, I haven't ventured west. I've got to Edinburgh twice and I think that's about it. Yeah.
Dr Jenna Macciochi: Yeah, it's beautiful. It's very wet. There's not a lot there. And we had a really small farm.
Dr Rupy: Sounds idyllic. I just imagine this farm to table food. Your mum's a professional chef, you're living off the land.
Dr Jenna Macciochi: Exactly. We're, you know, she taught me because because everything's quite seasonal, you know, we didn't have the variety of like exotic fruits and vegetables. It was really like what grew in that season and you had to have them.
Dr Rupy: Saying that, Scotland's got some amazing wild fruits, haven't they?
Dr Jenna Macciochi: Yes, yeah, and like mushroom season, we were all over that. Berries that I never see here, like tayberries, they're like these giant raspberries.
Dr Rupy: Tayberries? I've never even heard of that.
Dr Jenna Macciochi: Yeah. I just grew up thinking that was normal and then I came to down south and no one's heard of those.
Dr Rupy: I I come across this forager, I think it must have been on a TV program, like a cookery program, where he can mimic different exotic spices from all over the world, like coriander and Thai basil from herbs foraged in Scotland.
Dr Jenna Macciochi: Oh my goodness. I have to check that out.
Dr Rupy: I've got to look this guy up. I'll put it on the show notes, but it is incredible. And that that little snippet, I think it must have been on Saturday Kitchen or something. That little snippet really made me think, I've got to go to Scotland. I've really got to explore the different sort of culinary landscape.
Dr Jenna Macciochi: Yes, yeah. I mean, I think not always is the food is the first thing that springs to mind as being healthy. We have things like deep fried pizza, you know. But I think intrinsically, the kind of real traditional diet of Scotland, you can find that it is is relatively good for you. And it's, yeah, follows the seasons. And my mum taught me a lot of how to process, you know, when you have all your root vegetables coming at the one time, how do you store that so that they last over winter? And you know, how to just open your cupboard with hardly anything there and and suddenly make a meal from that. And I think those are great tools that that people need and perhaps have been lost a little bit.
Dr Rupy: Definitely. Yeah. You like me had a mother who was really into cooking and food and and trying different sort of types of cuisines and that being instilled generation to generation, I think is something that is becoming less and less normal.
Dr Jenna Macciochi: Exactly. I I can't help but think that there's something about the traditional way of life that we've lost. Like we very much were adapted to our environment because we had to be for survival. And it's kind of like the modern world is great, but have we thrown the bath water out with the baby or the baby out with the bath water? You know what I mean? It's like some of the elements of of how we used to live, perhaps might be quite useful now. And it's been a little bit lost.
Dr Rupy: I love using that evolutionary perspective and I think that's going to definitely come into our conversation with immunity today. But taking that perspective of like, okay, what are we adapted for? And how do we manage the advantages and the benefits of modern living with how we are designed to live both from a mental and a physical perspective as well.
Dr Jenna Macciochi: Exactly. I think when we unlock a lot of the secrets of evolutionary biology, it will yield a lot more in our understanding of why we are the way we are and then how to self-manage that to to fit in with the modern environment because that's not changing. You know, it's not going to go back to the rudimentary way of life.
Dr Rupy: Exactly. Yeah. I love that. And so you were based in Scotland and you came all the way down.
Dr Jenna Macciochi: Yeah, so for some reason as a child, I had an obsession with health and disease. I was just really curious about. Maybe it was living on a farm, you see the circle of life. You know, when I was thinking about what to do when I left school, I'd heard about immunology and there was a course at Glasgow University in the medical school where they just do immunology and it's very select, only 20 students. And I just thought, wow, this sounds really interesting. This sounds like this is the foundation of health and disease. And when I got there, I was like, amazing, I've found my people. This is what I want to do. And that was almost 20 years ago now. So I've just been in the field ever since. And I love it. And I think there's always more to learn.
Dr Rupy: Well, your passion definitely comes through on your blog, on your social posts and some of the articles that you've done as well for for major magazines. But let's get into it. So I think, and this is something we were talking about before the show, that the vernacular around immunology is very misunderstood and it's misguiding, I think, for a lot of people because you'll you'll find lots of articles like, you know, these are the top herbs to boost your immune system and you know, to to kill a cold and all this kind of stuff. So I think we should strip it right back and actually talk about what we mean by immunity.
Dr Jenna Macciochi: Yeah, definitely. I think that's really, that's probably what got me, you know, talking about this so much in the beginning, just hearing so much misinformation. And I think that the first thing to say that the immune system is this huge complex web that's all over our body. It's found everywhere in the brain, in all of your organs, in your blood. And people like to think about it as being a single on-off switch. So you want to switch it on, fight infections, you know, create this force field that's going to keep you well, and then switch it off again. And it's actually more like a series of different switches and you've got to have the right combinations. So it's a bit like a rheostat that you're constantly adjusting to get it just right. But then something in your environment will change, the season changes, and then you have to kind of tweak it again. So it's not just an on-off switch. I think that's probably a hang up from when people died from infection. And that's maybe going back 100 or so years ago. People might not make it to old age because they would die of infection that we don't see just now. So we're constantly thinking, we'll switch on our immune system, be invincible to infection. But it doesn't quite work like that. And it's important to say that immunity is what makes us unique. So it's almost like your fingerprint. Even in identical twins, their immune systems will be different. It's the way that the receptors are recombined. There's a really unique way that the genes work to make the the sort of repertoire of what we call our immune cells and all the different things that they can sense. So viruses, bacteria. So every one of us is unique. And there's a kind of fundamental reason for that because, you know, if if you think about a room full of people and you you throw in a cold virus, if they were all to get sick to the same degree, we'd probably have died out as a species by now. So there's there's a fundamental reason why we're we're immunologically all different because, you know, some people might be more susceptible to bacteria, some of us might be more susceptible to certain viruses or parasites. But if we're all the same, we wouldn't have survived. So there has to be that kind of uniqueness in our immune system.
Dr Rupy: I love that analogy actually, because that does tease out a lot about how one thing might not work for some person. That could be diet, it could be medications, it could be any sorts of things. And it might not do anything for the other person. And that uniqueness is something that I'm trying to bring out of people as well with the content I put out. It's about becoming the expert of not of health, of not of nutrition, but your own health and how that relates to you. So there's so much information out there, so much content, but really it's about filtering out that content and deciding how does that help me in this situation.
Dr Jenna Macciochi: Yes, exactly. And I think that's another, brings out another important aspect of the immune system is that it's always changing. It's not something that we're born with. I like to think of the immune system as something that's made. So you're born with a quite rudimentary immune system and you're relying on a lot of what you've got from your mother, both through the placenta and then if you're breastfed. And then your immune system really starts to develop from the moment that you're born. And it continues to develop and change throughout your lifetime into old age. So when people say, oh, I've got a really rubbish immune system, maybe at that moment in time because you've got a cold and you're feeling lousy, but, you know, it's not a fixed thing. There's things you can do to change it. And we know that only a fraction of what determines your immune system is in the genes. A lot of it is the environment, what you're doing. So things that you can actually be in charge of and manage by yourself. So nutrition being only one of those, but also all sorts of lifestyle factors.
Dr Rupy: Definitely, yeah. And we're definitely going to get into that. So your immune system essentially this complex set of cells. I think a lot of people don't realise that anything that really protects you and helps your your innate sort of homeostatic mechanisms, your your balancing mechanisms is part of your immunity. So that could be the acid in your stomach. It could be your nasal hairs in your nostrils. Your mouth and secretions on your skin. So it's it's cells, it's molecules, it's it's those barriers to infection. If you think about where you're normally going to get an infection, it's it's breathing things in or swallowing things or through the skin. It's the the bits that are exposed. And it's not just for infection. I think this is again something that people don't think about. It's also the main thing that's involved in repair and adaptation. So if you're going and and working out in the gym, your immune system's helping your muscles adapt, repair and strengthen. It's involved in pregnancy and the success of of carrying a child. It's it's really a key part of the aging process. It can really determine how well we age. And it's actually the main cancer surveillance that we have in our body. And I think that's again something that not many people think about.
Dr Rupy: Yeah. I I like to, I use the analogy in the next book, Eat to Beat Illness, about how your immune system, instead of being an aggressive military force, it's like a peacekeeper. It's sort of like looking at where there needs to be a little bit more action, a little bit more force, and actually where we need to step back a bit. Because an immune system that is overactive, that is boosted, if you like, is not a good thing.
Dr Jenna Macciochi: No, exactly. And that's where we lead to people who are suffering with autoimmune issues where your immune system essentially loses the capability to recognise friend from foe.
Dr Rupy: Yeah, exactly. I think that's really important. The immune system doesn't just recognise different pathogens, as we call them, so the bugs that are causing infection, but they recognise danger and damage. The immune cells are intimately entwined with all our other systems in the body. So they have receptors for your sex hormones, like estrogen, progesterone. So they're affected by different fluctuations in those. Also, they have receptors for stress hormones, like cortisol, and the neurotransmitters. So if you think about the complete picture, then how you're feeling, your stress, you know, the the different hormone times that maybe are going on, for example, in a woman's body, this is all affecting your immune system as well. So it's it's like the sixth sense, you know, it's really helping us manage our environment and and adapt to that as well.
Dr Rupy: I think that's a really good analogy actually, being the sixth sense. And already just from that description of just how complicated and intricate the system is, you can understand why just taking a single supplement is unlikely to be the silver bullet that magically improves your immune system to fight off a cold or whatever you're going through at that point in time. So I think that's like already, you know, a good understanding of why these things don't necessarily work.
Dr Jenna Macciochi: Exactly. When I when I start teaching immunology down at the University of Sussex, the first time that the students get any kind of insight, I show them this huge web of all the the cell populations and the sub-populations and then like the sub-populations. And you can just see, you know, the emoji of like the mind blowing because they're like, what? It's there's so many different things going on and so many switches that anything to do with the immune system is going to be multifaceted. So there's going to be a lot of different things going in to give you a certain result. So that's the reason that there's not going to be one single supplement or thing that you can do that's going to give you some kind of immune effect. It's always going to be multi-pronged in your approach.
Dr Rupy: That description of all those different sort of immunological factors brought back loads of painful memories for me actually in medical school trying to figure out, oh God, like all these different like T-regulatory cells and MHC complexes, like what is going on?
Dr Jenna Macciochi: Every year they discover a new subset or a subset of a subset. And then there's like the complement system, which is just like.
Dr Rupy: I actually had some people message me on Instagram and social media just saying, can she just describe exactly what a complement is and what is MHC? What are all these different sort of immunological factors? You know, it's quite funny actually. There's a lot of medical students I think that follow me and they're just trying to get like answers for their essays.
Dr Jenna Macciochi: I always think I'm I've got to work really hard not to scare people off immunology in the beginning because it does get really interesting later on.
Dr Rupy: Yeah, yeah. So now we kind of understand what the immune system is. And you're suffering from a cold at the moment.
Dr Jenna Macciochi: I know, ironically. Somebody said to me the other day, like, I didn't think you would get sick. You're always talking about the immune system. Surely you should be invincible.
Dr Rupy: And this is something I talk to patients about. It's like, the very fact that you're sick and you have a temperature and you, you know, you have all these other sort of, you have a cough, you have a tickle, you have a throat sensation, shows you that your immune system is actually working.
Dr Jenna Macciochi: Yeah, exactly.
Dr Rupy: And it's about changing your perspective from one that is annoyed by the fact that you have a cold, which is, I I get it, it's super annoying, but you should also be grateful and appreciative of the fact that your immune system is working. And not everyone has an intact immune system that can tolerate that. And you're most likely going to be fine in a couple of days.
Dr Jenna Macciochi: Yeah, that's the thing. Colds and flus are self-limiting. There's so many different varieties, which is why it's normal to get a few every year. And most of the time we don't even realise your immune system's working. I mean, we live in this really microbial world and every day it's just like fending things off. We don't even notice it. And every now and again, one might slip through the net and then you get sick. And the symptoms are actually your immune system more than the actual infection in most cases. So they might be unpleasant, but you've just got to ride them out. And this is again where I think like modern life is hard because, you know, the general message is like, go down the pharmacy, buy all the over the counter medications, and then get to work and struggle through the day. And if you actually maybe just took a day off or two and rested, you'd probably get over it a lot quicker.
Dr Rupy: Exactly, yeah. Our producer's actually were talking about some cold and flu over the counter medications. I was like, oh, what do you reckon about this one? I can't remember what it was. It was some spray for the back of your throat.
Dr Jenna Macciochi: It's really funny. Even though I tell this to my husband all the time, he loves himself one of those like, you know, the you put the hot water in and it's like a paracetamol based like decongestant thing. I'm like, that tastes disgusting. Save your money.
Dr Rupy: Yeah, I know. Yeah. We'll talk about that actually with the the fever sort of balancing medications and stuff. But now we know how complicated the system is and it's basically everywhere. Are there any particular sites where the immune system will dominate?
Dr Jenna Macciochi: Yes. Well, I think the one that you can't escape is is the gut. And I think there's.
Dr Rupy: It wasn't long until we're going to start talking about the gut.
Dr Jenna Macciochi: Yes, exactly. You you can't not not talk about the gut when you talk about the immune system. They are completely dependent on each other. And it's that dinner party fact of like, oh, did you know most of your immune system is in the gut? Well, it's true. And there's good reason for that. I think with a lot of things in biology, the the form follows the function. So the the the structure of the digestive tract, the whole architecture, it's optimized for digestion to get the most out of your food. That creates a vulnerability because it's actually the lining of your digestive tract is only one cell thick. So to me, that's like quite fragile. You know, there's there's all sorts of things going into your mouth every day. There's just the general bacteria and and bugs that are in our environment that we're swallowing. There's things that could be in our food that could make us sick. And just the food itself, how does the immune system know not to respond to that? So because of that, there's maybe about 70 to 80% of your immune cells that line the the digestive tract and they form all these kind of unique structures that have unique ways to keep a surveillance on what's going on. So that's really quite important.
Dr Rupy: Yeah, absolutely. I think that that sort of the the very fact that the architecture is only one cell thick shows you why it's so important to have your immune cells there. Because we're in constant communication with our environment via our 30 cm long digestive sack, or the first part of it anyway. And and that's why, you know, it's it's just a natural evolution as to why we have immune cells in those areas.
Dr Jenna Macciochi: Yeah, exactly. Yeah. And and, you know, I think it's such a portal for infection, you know, that we have to have those defenses there. It's interesting then to talk about the microbiome of the gut. This is getting a lot of air time. People are getting more aware of the microbiome. And what we do know that if you do not have a microbiome, then your immune system does not develop. It's it's completely reliant on the colonization after birth of our microbiome to develop fully. So I think that's another reason why we should take care of our gut microbiome.
Dr Rupy: Yeah. It's one of those reasons why we're seeing with C-sections and versus natural delivery and those babies who have C-sections are more at risk of having atopy, so allergic reactions and issues like asthma and eczema and stuff like that. Not to say that that's a definite, you know, it's a definite case study that you're definitely going to get asthma, but you're certainly more at risk because of the issues with poor microbial development in the in the gut.
Dr Jenna Macciochi: Yeah, exactly. And there's a lot of work trying to unpick those mechanisms because I think that's going to be really important to understand. That leads quite nicely on to the point that much of your immunity is actually set up in childhood. So many people who might be thinking, oh, I've got a terrible immune system, perhaps there are elements of what happened in those very early years that have had downstream consequences. And I think it's always helpful to think about what you can affect and, you know, instead of focusing on, oh, I was a C-section baby or I wasn't breastfed or these things, it's, you know, you can't change those. So it's better to think about what we can change.
Dr Rupy: Exactly. It's I have a lot of patients actually in general practice who over the last 20 years of their life, young patients, 20 or 30 years old, they had recurrent illnesses as kids. And you can almost map a pattern with antibiotic use and C-section and not breastfed and all the other factors beyond just nutrition and medications that may have led to them having issues with their gut or issues with eczema, dry skin and a whole spectrum of different diseases because of a poor microbial environment. That isn't to say that they are they're sentenced to that for life, but there are certainly things that we'll end up talking about about how we can actually encourage microbial development.
Dr Jenna Macciochi: Yeah, you might just have a different set point because of those early events that happened because you're you're more or less sterile when you're born. And then you're subsequently colonized as soon as you enter into this microbial world. And it's it's useful to think of it as, you know, the microbes were there before us. So we've evolved with them. We have to find a way to sort of have a a mutual relationship. So they actually do quite a lot for us in the gut. They themselves are part of our immune defense. So we we talk about the microbial barrier. Because they out compete with any bad bacteria that could be coming in through the mouth and not giving them any space. And they also make sure that that delicate barrier of our gut is really strong and really tight. And this is an area of where I used to actually do a lot of research on when I was in Switzerland is this whole idea of leaky gut, which I think is one of those kind of woo-woo terms.
Dr Rupy: It is, yeah. It's it's it's weird because if you type in leaky gut into like PubMed, you you won't get much. But if you type in intestinal hyperpermeability, that's when you get, oh, okay, there is actually a lot of science behind this. Yeah.
Dr Jenna Macciochi: Exactly. The the scientists have sort of always been there and I guess the leaky gut term kind of existed in a parallel woo-woo world and now the two are kind of converging and it's.
Dr Rupy: So you've actually done some research in this?
Dr Jenna Macciochi: Yeah, so that was a lot of the work when I I worked out in Switzerland. Trying to understand, so I actually worked for a pharmaceutical company. I wasn't making drugs, but they employed me to try and understand what was going on in a normal situation in the gut in terms of the immune system to try and figure out, okay, what happens when that's perturbed and then can we intervene with something. So they were kind of hoping that I would give them some drug targets, but I was just like, oh, this is amazing. I can unpick the science, what's going on. And sometimes you have to know what's happening in a normal situation to know how that goes wrong.
Dr Rupy: And in a normal situation, those tight junctions that exist between these one cell thick lining, they they increase and they decrease, right? They become more leaky and they become less leaky. But that's normal.
Dr Jenna Macciochi: That's normal. I think that's a really important thing to point out because people can get very confused if they start Dr. Googling leaky gut. But it is a normal physiological phenomenon. There's actually certain components of our diet that can exacerbate that leakiness. The two really well-known ones are are fat, in particular saturated fat, and the fructose from fruit sugars. But that's not to say that we should avoid those things because there's actually a lot of evidence that if you're consuming fat or saturated fat or fructose with fiber and with phytonutrients, that is actually fueling the bacteria in your gut, your microbiome, to produce particular things, short chain fatty acids being one of those, that helps seal up the gut again. So it's actually quite useful to open the gut when you're digesting food to facilitate the whole digestion and getting the nutrients into the body. And then the fiber helps to shut it back up again.
Dr Rupy: So would you say it's less about having a leaky gut or having permeability of your gut and more about the timing of how long you expose those tight junctions to be open essentially versus closed?
Dr Jenna Macciochi: Yes, I think that's the picture that's starting to emerge. And that I think ties in quite nicely to dietary patterns rather than focusing on specific nutrients. So how many times a day we're opening up the gut? And one of the reasons that opening the gut up is is detrimental for the body is because the the microbiome that lives inside our gut can slip through those holes into the bloodstream and all around the body. And while those are considered our good bacteria because they live in the gut and they do a lot of good things for us, when they get in the wrong place, they're just the same as any other bad bacteria. They have the same molecular patterns on them that send an alarm signal to the immune system. They switch on inflammation. And this can all be happening at a sort of low level that you wouldn't perhaps even be aware of. There's sort of no firm signs and symptoms of this going on. But I think cumulatively over a long period of time, then it could be that we start to see some some damage going on and and things springing up.
Dr Rupy: It's it's I think it's quite important for for the listeners to understand that your immune system is very much related to the inflammation response. And it's essentially mediated by the immune system. So when you need to have a response to a bacterial infection, a virus, or or even normal colonization of of your gut, it will elicit this inflammatory response. And I suppose it goes back to this timing. It's like, okay, you can have a little bit of an inflammation when you eat because that is very normal. But when you when you're eating for long periods of time, so actually when you're grazing or when you're having the wrong sorts of foods and it's this constant sort of exposure, that's when you have this low-grade inflammation, meta-inflammation in the literature, that can lead to ill health outcomes.
Dr Jenna Macciochi: Yes, exactly. And I think the one key thing maybe to talk about with regard to inflammation is that it's it's acute by design. So it's only ever supposed to be a short-term thing. And then if it's happening all the time, it starts to take its toll on the body. And we we call it chronic, so it's a more of a long-term thing. But yeah, the the leaky gut thing, I think people shouldn't be concerned about. It's normal. But I think that you there's things you can do to prevent leaky gut. And fiber and phytonutrients are two of the proven ways that we know help tighten it up again.
Dr Rupy: You're sorry.
Dr Jenna Macciochi: I was going to say it ties in quite nicely with some of the work that's coming out about time-restricted eating and consolidating eating into certain times of the day rather than the the snacking constantly because eating is is inflammatory. And again, that's normal, but you don't want to be doing it all the time because it's just another load that your body has to deal with.
Dr Rupy: Absolutely. When I talk about eating being inflammatory, it just raises a lot of alarm bells whenever it's like eating causes inflammation. Everyone's like, what?
Dr Jenna Macciochi: I think about everything through like the scientific lens. So to me, it's it's normal because I know what I mean, but I think when you say it to other people, they're like, you know, it's not that you shouldn't eat, but maybe think about how you're eating. And again, I think it just plays into modern life. Like, it's hard to sit down and have a meal. And it's, you know, everything is rushing. Everything around us tells us to snack. So I I lived in Switzerland for for a long time and I came back to the UK two years ago. And I was kind of like, this is everything is pre-packaged into little things telling you that you need to eat on the go. And that that doesn't really happen in Switzerland. I found it quite a strange observation, like coming back to the UK and and you have to also think about the environmental impact of that because they're all wrapped in single use plastic. Like, do we need to have so many little snack bars and snack pots and you know, everything.
Dr Rupy: I think that's one of the many factors that could potentially explain the French paradox. So everyone looks at the macronutrient combination, oh, they have loads of saturated fat, they have loads of, you know, meat in their diet. But actually, they spend an hour for lunch. And this whole concept of grab and go sandwiches is just not there. And I think the process of eating and the sense that they get around lunchtime being their time is very telling for why they might have lower rates of cardiovascular disease and and other diseases.
Dr Jenna Macciochi: Definitely, despite having some of the dietary red flags. I I really noticed this in Switzerland, which again is a country that has really good health span and it's it's a different setup to the UK, so you can't really compare, but I was working for a large company and they had this huge campus. And at 11:30, the Swiss all start really early. At 11:30 every day, they troop down to the the different restaurants and stuff on the campus to have lunch. And everybody ate together and lunch was like one hour, one and a half hours. And the canteen was only open between like 11:30 and 1:00. So you had to eat in that window. And and you know, my colleagues were having like a rosti, which is like the fried potato covered in cheese with a fried egg on top, bacon, and there would always be some dessert or cake, then coffee. But it was like a whole like process. Everybody got away from their desk. And in the beginning, I found this like, I can't eat this for lunch. Sounds like Christmas lunch every day. Exactly. But you know, none of my colleagues were very unfit or, you know, looked overweight or, you know, everybody was very active as well. It was part of the culture and the lifestyle, but I think it's, yeah, the snacking culture has not served us well. And it's hard to kind of put your finger on what it is about it, but I'm really convinced that this is not helping us in some sense. And if we can get back to something a bit more traditional, a bit more boring, maybe it's going to be a bit useful.
Dr Rupy: I think using that evolutionary perspective about around time restricted eating or as I like to call it, defined periods of eating. It sounds a little bit less intrusive and a little bit less like restrictive, exactly. But some really interesting research coming out from the West Coast of America looking at time restricted feeding where you don't change the calorific content of your food at all. You just change when you eat it. It's a very actionable tool for a lot of people. And it's something that I talked about in my first book, The Doctor's Kitchen, but also my second book, Eat to Beat Illness, where, you know, that as a principle of healthy eating, just the timing of food is something that could potentially have very good effects.
Dr Jenna Macciochi: Yeah, exactly. I think we're just so over the time of restriction. Like adding that restriction onto your life, if you're trying, oh, I'll only have this really low calorie salad that's not going to satisfy me for lunch and leave me just thinking, oh, I want to eat all the food all afternoon. I think that it's not it's not been helpful and we have to move away from that and start enjoying food. Definitely in terms of the immune system, there's evidence that endorphins are really helpful in how the immune system works. So if you're going on holiday and you find that you might have, if you have an autoimmune disease or an allergy or some kind of food intolerance, it might suddenly become a lot better when you go on holiday. And you just attribute that to eating a different kind of food, but it might be because you're happy when you're eating and that actually boosts these regulatory T cells that we have in our body that that sort of gently tap the brakes on the immune system and keep it in check. So I think there's a lot to be said for like, you know, how you're feeling when you're eating and what you're doing in your day-to-day life. So managing the stress.
Dr Rupy: Even on an anecdotal level, like, you know, I have patients that come in and they're they're they're stressed at work, they're working long hours. Obviously, there's there's loads of confounding things in the fact that they're probably reducing their sleep, they're probably not eating right. But certainly stress having an impact on the likelihood of you having a viral illness, it's certainly there in my opinion.
Dr Jenna Macciochi: Yes, definitely. Yeah, no, there is there is evidence to to suggest that. I mean, in the short term, actually stressors are quite useful for the immune system. They clear out a lot of inflammation and they can actually get rid of a lot of old and aging cells and give space for new cells. Because we have this concept in immunology of the immunological space. So you can only have so many immune cells in your body at one time. And as we get older, they start to age. You want to get rid of some of the old ones, bring in some of the new ones. And stressors like running away from something and and or some really short intense exercise or something that's quite stressful but very acute, that can actually be quite beneficial for the immune system. But when it becomes either a chronic long-term stress, so you have to care for a sick relative or or short intermittent stresses, so lots of frequent times when you're becoming stressed, it's maladaptive. So the immune system actually becomes less responsive to that cortisol effect and you lose the benefits of sort of more acute stresses to the overall health of the immune system.
Dr Rupy: I've I've been coming across a lot of research looking at fasting as well as time restricted eating and its impact on the immune system through the lens of not only autoimmune issues and diabetes in terms of therapeutics, but also cancer as well. Which I think, I mean, first to caveat it, it's there's very small research studies. It's it's very, it's not practice at the moment. It's not in first line practice. And obviously, a lot of people who have issues around eating and disordered eating shouldn't certainly not engage in any fasting practices. Having said that, it is quite interesting from an immunological perspective.
Dr Jenna Macciochi: Yes, definitely. I think the research coming out is really exciting and I'm really curious to see how that evolves. It is very experimental at the moment. But again, fasting is considered another stress on the body. So the immune system is highly dependent on all nutrients. So all the macros, it needs protein, carbohydrates and fats and all your vitamins and minerals. These are all necessary to help the normal running of the immune system. And they're really good at sensing nutrient status. So they they know what's going on and they can respond appropriately. And different nutrient sort of profiles in the body or metabolic profiles can seem to influence the fate of immune cells to go down either more regulatory paths or more inflammatory paths. So it seems to be like manipulating that could help redirect the immune system away from being quite an autoimmune phenotype. So help people with that. Also, fasting in itself will kill off any vulnerable immune cells. So as they age, they're more likely to go wrong. Like anything with time, you know, as your car gets older, it's more likely to be a bit faulty. And sometimes there is a time where you've just, you know, it's it's it's time to change the car. Exactly. Get rid of that. And and things like fasting, so reducing nutrient availability makes those kind of older cells a bit more vulnerable and they're more likely to pop and go through apoptosis, which is this process that removes them. And then you have more space to repopulate with new immune cells.
Dr Rupy: I I like this because there's lots of arguments for and against it, right? So the process of fasting, upregulating autophagy, which is the self-regulation where you clear out the old dead cells, senescent cells that are sort of like hanging around, they don't really do much, they're not really functioning, but they're more likely to go wrong. Exactly. And they emit like mild inflammation signals and you know, that that can be. So clearing that is is great. And then also going back to what we were talking about where you essentially give your gut a break from digestion, the tight junctions, that can also reduce your immune cell response. But then also, conversely, if you're not eating, then your bacteria are not being provided with a food source and they could essentially start damaging the lining of your gut. So everyone's like, what do I do? Do I fast or I not fast?
Dr Jenna Macciochi: Exactly. I think it's finding that sweet spot and we don't we don't know what that is. Yeah, so the I think the microbiome is a really important point because your your gut is lined with mucus, which is essentially like a kind of carbohydrate source for so if they haven't got any food, eventually they just start eating the mucus, which is part of our defense as a barrier. And then once that goes, your your gut lining is more vulnerable. But there's definitely a window whereby fasting is having the beneficial effects before it tips over into the more negative effects. And there's a lot of speculation as to how many hours or days that you should be fasting to give you this sort of reboot. And I think the truth is that we don't know conclusively and and we're not able to sort of dish out that to patients or the general public yet. But I think there's a lot of trials and a lot of a lot of things are going to come out in that area.
Dr Rupy: There's a lot of self-experimentation I'm finding of researchers themselves who are trying to experiment with with fasting. I haven't done it yet myself, but I'd be super interested to see what the effects are, but actually conduct it like an experiment. So measuring my my vitals before and after and some inflammatory markers and the rest of it. But I think it's going to be really, really hard just looking forward to demonstrate what the sweet spot is for the general population.
Dr Jenna Macciochi: It might be quite a unique thing, individual to the person. The age of the person might be quite important as well. So as well.
Dr Rupy: And that's before we even think about like the mental health impact as well of like declining yourself to have food when there's so much food around. And that could potentially for certain people serve to increase your cortisol response, increase your stress around food and actually lead to an overall negative effect, which is something you have to balance. But that's why I'm just a big fan of the defined eating periods.
Dr Jenna Macciochi: Yes, yeah. I mean, that's something I've been doing for quite a long time now. And I do it with my kids as a practice of getting them used to knowing what a meal is, that we sit down and we enjoy our food and we talk and it's it's family time, rather than being like, oh, you only eat at these times of the day, but they know what breakfast, lunch and dinner is and gently kind of not put them in a situation where they think it's normal to snack all day. So it's kind of making meal times like a happy time that is for everybody.
Dr Rupy: Because there was this myth, wasn't there? Like, you know, if you graze a little bit throughout the whole day, it'll increase your metabolic energy and it'll reduce your weight and all the rest of it. But generally what I mean by defined eating periods are anywhere between 10 and 12 hours in the day where those are the times when you eat and everything around that you try and keep clear. Obviously within reason. For example, today's Friday, I'm going to go out for dinner with a couple of my friends that I haven't seen for about a month. And we're going to eat.
Dr Jenna Macciochi: Yeah, exactly. Yeah, Wednesday night I had a Christmas party and you know, I was eating dinner way later than normal because I normally eat with my kids, so it's quite early that they have dinner. But you know, that's that's the thing, the beauty of doing everything most of the time that you've got that buffer for, you know, when you let your hair down.
Dr Rupy: It's interesting. Recently I was writing an article around this whole hypothesis about the inflammatory load of the gut. And I was trying to find out why we have these guidelines to eat little and often and this dogma that is really in people's heads that they can't go more than three hours because, you know, like something terrible will happen if I don't get food. And I was trying to figure out where that had come from, what it was based on. And most of it was just kind of assuming that we could stabilize insulin levels by, you know, having the food kind of little and often. And there was no sort of hard fast evidence on any other reason or why that sort of evolved. And it's just one of those things that people must have thought that seems sensible. And no one ever stopped to think whether that is actually the best guideline.
Dr Jenna Macciochi: It's really strange because actually if you look at some fasting studies, and I think they go back really far because it's quite unethical to to maintain fasting for these patients. But they would go weeks and weeks of of just not having any food and they were maintaining a glucose level because you essentially go into a state where you start burning your fat. But then when you're running out of fat, you're also burning your protein. So you're maintaining a glucose level because glucose is fundamentally one of the most important fuel sources for all of our cells in the body. So even if you're not taking in glucose, your body is still adapted to having a glucose level. So this whole process of like eating little and often to maintain a glucose and an insulin level that's low, like it doesn't doesn't seem to make sense.
Dr Rupy: And then well, if I if I haven't eaten, then I I have energy stored on my body. My body just needs to know how to use it. And that's an adaptation and that, you know, it's something that you need to to be able to do. And yeah, I think we've kind of lost touch with our intuition about eating. It's something I definitely noticed moving back from Switzerland to the UK. There everything felt quite intuitive. You know, people were eating these huge lunches. And I remember saying to my colleague Sven, like, you know, what do you what do you have for dinner? And he's like, well, you know, in winter, I'll have maybe a soup. And then in the summer, maybe a salad around like 5, 6 o'clock when he got home. But he'd had this huge, huge lunch. And there was there was nowhere to snack in the in the whole campus. You know, there was maybe one or two vending machines that you could find somewhere when in, you know, that would have food available. But the the restaurants and the canteen were just literally open during lunch and then shut again. And it was kind of just like, that's normal because that's lunchtime. And there was not the kind of grazing.
Dr Rupy: It's definitely not like what it's like here. There's like 10 stores where you can get any sorts of food.
Dr Jenna Macciochi: And I just think you have to cut through the noise and think, what are my needs? Do I need all these little plastic pots of snacks all the time or, you know, can I wait till lunch and have something substantial that's not going to make me feel like I want to eat again before dinner?
Dr Rupy: I'm sure you'll agree that was a super in-depth look at the immune system and we're not done yet. So make sure you subscribe to the Doctor's Kitchen to make sure you don't miss the second part where we talk more in depth about the actual foods and lifestyle practices that are going to be exceptionally important for supporting your immune health. If there's any recipe that I can actually advise on the basis of what our discussion was today, it would be the medicinal broth from the Doctor's Kitchen book one. It's a fantastic, easy recipe to make, particularly if you're feeling a bit under the weather, and it has all those different polyphenols and variety of colours that will support your immune system. You can find Dr Jenna at drjennamacciochi.com, also on Twitter @DrMac and on Instagram @drjennamacciochi. She's got some great articles on her website. I highly recommend you check those out and they will be on the show notes on the doctorskitchen.com. Make sure you subscribe to the Doctor's Kitchen and give this podcast a five-star review. It really does help people who might need the information find it on iTunes and all your other podcast players. See you next time.