Dr Rabia: You can go down the investigative route and it will lead you down a certain path. But what for me, I think the conclusion I've come to in the last sort of eight months is that breathing in the lab is very interesting, but actually in real life, there is no doubt that it has positive effects.
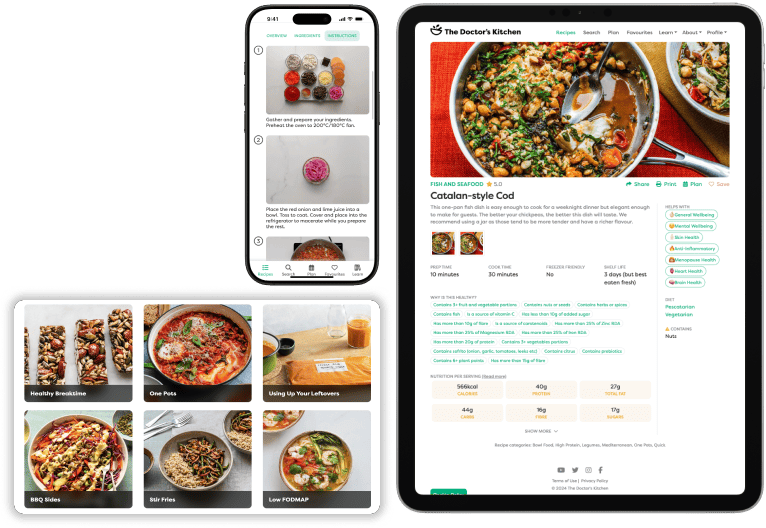
Dr Rupy: Welcome to the Doctor's Kitchen podcast with me, Dr Rupy, where we discuss the most important topics and concepts in the medicinal qualities of food and lifestyle. Today, I'm speaking to the incredible Dr Rabia Lalani, a gastroenterologist and clinical research fellow at the Wingate Institute of Neurogastroenterology from Queen Mary's University. Dr Rabia is in the process of creating a guide using slow deep breathing techniques with audiovisual biofeedback for relief of anxiety and digestive discomfort. And on this pod, we will be discussing the gut-brain axis, functional gut issues and what that means, that actually includes IBS as the most common one that people know about, and how stress in particular impacts our gut health, living with gut issues and the impact of lifestyle interventions such as breathing. You'll find the recipe video that I cooked for Dr Rabia at the start of the show on my YouTube channel, The Doctor's Kitchen, so you can see how delicious and easy it was to make, even whilst recording a podcast. You can find all of this information and more at thedoctorskitchen.com. Subscribe to the newsletter for weekly science-based recipes and listen to the end of the pod for a summary of our discussion and how we can potentially improve our gut health using lifestyle techniques. On to the podcast. Dr Rabia, welcome to the Doctor's Kitchen.
Dr Rabia: Thank you for having me.
Dr Rupy: No worries, no worries. So, like I said before, I've misguidedly decided to cook you a hot brunch on one of the hottest days in London today.
Dr Rabia: It's all good. We will survive.
Dr Rupy: So you've got an allergy to nuts and seeds, so we haven't done any of that, which I usually put in, unfortunately. I usually put in nuts and seeds for the fibre and the quality fats.
Dr Rabia: Sorry about that.
Dr Rupy: No, no, no, that's cool. We've got loads of good fats coming from the extra virgin olive oil. So I'm going to be making you a savoury oats dish.
Dr Rabia: So good.
Dr Rupy: A lot of people shudder at the thought of a savoury oats dish, but honestly, it can be very delicious. A lot of Sri Lankan food has, or South Indian food, have you heard of poha? It's like a flat rice grain. It kind of looks like oats, but it's quite hard to get in the UK. But oats is a very good sort of substitute for that. And it gives the same sort of flavour. So we're making savoury oats with some mushrooms, sun-dried tomatoes, tarragon, a bit of spinach, and bring it all together with a little bit of veg stock. Sound good?
Dr Rabia: Perfect. Sounds so delicious. I'm so excited.
Dr Rupy: We're just going to toast these oats in a dry pan before we get everything cooking.
Dr Rabia: So it's just dry toasting?
Dr Rupy: Dry toasting for now. And what dry toasting does is it just brings the flavour out of the oats itself. It also reduces the cooking time because we're not going to cook it like you would traditional porridge oats with loads of milk or water and then put a lid on. It's quick cooking in the extra virgin olive oil. Hopefully the flavours will marry all together.
Dr Rabia: Nice.
Dr Rupy: I'm so good. So, Dr Rabia, you, I'm going to call you Rabia now. It's too much.
Dr Rabia: Yes, please. Please. Take off the formality.
Dr Rupy: Your research is what brought us together. We were introduced by, was it Dr Professor Tony Young? Did he connect us on?
Dr Rabia: Yes. So, well, no, actually, he was doing a evening entrepreneur session for NHS entrepreneurs, which you're a part of now. And one of the pit stops. Yes. So I went along just a friend of a friend and he mentioned you as somebody to connect with and share ideas in this space. So I actually got your recipe book off a mutual friend of ours. And I literally emailed your email address, like Doctor's Kitchen, and got a response and just said, can we go for coffee? And I was surprised to say you said yeah, and then we just sort of took it from there with your busy schedule. So, yeah, we kind of did it that way.
Dr Rupy: Well, I mean, when you, when you emailed, I remember now, I was absolutely fascinated by what you were talking about because I've never heard of neurogastroenterology. So actually, for the listeners, what is neurogastroenterology? What is your sort of your field? How did you even get there?
Dr Rabia: Okay. So, it needs a bit of explanation. Take your time. So, yeah, I'm a gastroenterologist, which I think sort of means that my beloved organ is the gut and the liver and the pancreas. And I have a hard time explaining that to friends because they don't understand why I'd want to spend my whole life looking up people's bottoms and why I couldn't choose a more sexy organ like the heart or something. But anyway, it's easier to explain now because as you know, the kind of gut-brain axis has become so trendy these days.
Dr Rupy: Absolutely. Yeah. Everything's to do with the gut, aren't they? People are talking about their poo more than often now.
Dr Rabia: It's completely boomed. And I'm really hopeful that the stigma is going down. I think we've got a long way to go, but I think the wellness sector and everything has gone a long way to improve that. So how I got into neurogastroenterology, which is, as it says on the tin, it's neuro, brain, gastro, gut. So it's the all the study of the brain-gut axis, which now in the literature has been redefined to brain-gut-microbiota axis. So that's the kind of new term these days.
Dr Rupy: Okay, I didn't know that.
Dr Rabia: Yeah, so it's now BGM or whatever. So I was sat in clinic, as a young registrar, as you'll be familiar with, and I just noticed that about a third of the patients coming into clinic didn't have a problem with the structure of their gut, right? So we would look up them, we look up the gut with a telescope and we couldn't see any problems with them, but they had significant symptoms. And I just felt that about, you know, a third of patients, I would just turn away. I would say, well, there's nothing coming up on your tests, they're completely normal. The endoscopy is normal and you need to go back to your GP and do X, Y and Z. But I knew for a fact, because these patients get re-referred, that they really are not getting a satisfactory service back in the community. And it's such a shame. But they were coming back and then I was spending that little bit longer to investigate what was going on. And it all came back to this idea that there is this complex interaction between our environment, our personality and our modern lifestyles with the gut. So I came across this as a specialty and I was so chuffed because it is a subspecialty. It's only practiced in two centres in the UK. So it's at the Wingate Institute of Neurogastroenterology attached to the Royal London in East London and also UCL. And I work with Professor Qasim Aziz, who is one of the leading neurogastroenterologists in the UK. And he's my supervisor. So he actually...
Dr Rupy: I remember looking him up actually when you told me about him. Yeah, yeah, he's done some phenomenal work.
Dr Rabia: I don't think people have heard much about him, but he's, yeah, he's gone a long way to improving the field. So, I, he actually, I started going to his clinics. So as a reg, I would just go maybe once a month, get some study leave, turn up, see what he was doing.
Dr Rupy: Oh, so you were going in your own time?
Dr Rabia: Yeah.
Dr Rupy: Oh, wow. Okay.
Dr Rabia: I mean, I suppose it's the starting point to any interest. So I would just take leave, go there, sit in on his clinic, observe him, watch what he was doing.
Dr Rupy: Oh, you must have loved that back in the day, right? Because it wasn't a very sort of sexy field back then.
Dr Rabia: No. I still don't think it's that, I mean, certainly within the medical field.
Dr Rupy: Sure, yeah. I think we're on the cusp, definitely. Yeah, but...
Dr Rabia: That smells gorgeous, by the way.
Dr Rupy: Oh, great. Good. Does the tomatoes going in, it's like reached the centre of the room.
Dr Rabia: That's why I use sun-dried tomatoes quite a bit because it imparts so much flavour for just one ingredient. So just for the listeners, what I've done thus far is put the oats in, toasted those, added a little bit of extra virgin olive oil, gone in with the finely chopped shiitake mushrooms and some of the sun-dried baby tomatoes, which have a natural sort of oregano flavour to them as well. Chopped up some tarragon that I'm going to throw in a bit later. We're just going to let this cook for a minute or so and then add some vegetable stock to essentially cook the mushrooms a bit more and the oats and then we'll bring everything else together. So...
Dr Rupy: So good. You're going to write all this down for me, right? Because when I want to replicate it.
Dr Rabia: It will be on the podcast notes on thedoctorskitchen.com, so everyone will see this recipe and your reaction to it as well. Hopefully it's a good one. So you were at the Wingate Institute, you were volunteering, going, hanging out with Professor.
Dr Rupy: Exactly.
Dr Rabia: And all the while I'm sort of doing my day job, seeing these patients, feeling reasonably dissatisfied. And then popping into his clinic, doing some observation. And then I decided, okay, what I need to be doing with my career is setting up a service in the future, something that sits in the sweet spot between what mainstream medicine is doing and what is happening in the kind of complementary lifestyle sector. And there is a sweet spot and I think it's unfilled. So I was wondering how I was going to go about that. And I actually applied for a management job in the NHS. And I had, I got the job and I was waiting to start. So this is like two weeks before start date. And I receive a call from Professor Aziz and he says, a position has opened up at the Wingate, to be a researcher, actually running a trial, will you come and work with me? And it's just something I couldn't turn down. So come September 2018, I started work there as a researcher and here I am.
Dr Rupy: Absolutely. That's great. Lots of ideas. Yeah, definitely. So that sort of convoluted path. And you went straight into gastroenterology, I'm assuming?
Dr Rabia: Yeah, yeah. So studied at Bristol and then, yeah, straight through. Straight through. And so you never thought that you'd be going down the neurogastro route and looking at sort of all this sort of, how, what was your introduction to wellness? Was it the dissatisfaction that you were having with patients that you sent back to the community, they didn't get good sort of treatment, they would always come back? Was that sort of your entry into wellness or did you have sort of any personal interest in into lifestyle medicine or?
Dr Rupy: Yeah. So, I think in order to see that as a problem, you have to have the certain pair of glasses on, right? To see that patients are reasonably dissatisfied. So those glasses came probably as my training as a yoga teacher, I would say. So I was doing yoga for many years in Bristol and then qualified a couple of years ago as a Ashtanga Vinyasa teacher.
Dr Rabia: Fantastic.
Dr Rupy: So I think I've always had that interest, you know, in how can we bring a more holistic viewpoint to gastro care. So I think those are the glasses I was wearing from like day one. And then these patients started coming in and I just thought there has to be something that we can do. And I don't know what that is yet. So watch this space. But I'm very keen to share my ideas around it because it's not just for me, it's for, it's for all clinicians to sort of kind of jump on that trend, I think, that's going that way.
Dr Rabia: So I remember actually one of the first questions you asked me was like, how are you managing the sort of complex interplay between lifestyle medicine, traditional medicine and that kind of quirky stuff that's on the cusp of, you know, evidence-based and, you know, whether we should be even talking about that because that's kind of what shrouds a lot of issues that we have as lifestyle medicine practitioners, you know, people talking about food and medicine can be talking about food as a cure-all and as a pill versus food as an adjunct to conventional therapy, which is what I believe in. And there is a lot of evidence based in. So, you know, there is this uncomfortable line that we as practitioners have to have to test and we have to walk. How has it been for you thus far?
Dr Rupy: Yeah, challenging. And that is definitely what one of the things that really attracted me to, you know, collaborating with you is the way that you've done your recipe book with all the references and everything because as conventional doctors, we, you know, we have to follow that evidence-based line for a good reason. And I think what I used to call the complementary and alternative sector, I then started calling lifestyle medicine because what I realized is that certainly in our lifetime, we're not going to be able to completely validate complementary health.
Dr Rabia: Absolutely.
Dr Rupy: And therefore, we are never going to be able to stand as doctors conventionally trained and say that we can recommend X, Y and Z to our patients. Not that, not that it cannot complement it, but that we can't necessarily always recommend it because it's completely bespoke and personalized for the individual. And that's not how evidence-based medicine works. We work on trends and we work on large cohorts of patients where we prove that a certain significance in results. So I'm that's how I came to the lifestyle medicine idea because I can see how that is the go-between of complementary alternative health where patients often get lost. I mean, they go into that sector, they can spend so much money, they don't know what they're buying, but they're desperate. And I don't blame them. So we need to shine some light on that for sure. And I think hopefully, you know, you and I are going to be part of that and you've already, you've already done it. So I think I think it's like shining light on that and then talking about lifestyle medicine as the go-between.
Dr Rabia: Absolutely. You know what? I remember having these sort of thoughts when I was a medical student as well. One of my early mentors was a gastroenterologist at Charing Cross, fantastic gastro physician, amazing person, very, very caring. But I remember being in a consultation with him and we had a young woman, lawyer, who had functional gut issues for many years, been tried on a whole bunch of different medications. She ended up leaving the consultation with some Domperidone. But she'd had all the investigations that, you know, we're talking about scopes and blood tests and x-rays and a whole bunch of other things and no sort of cause found for her issues. And then she was just sent home with the Domperidone prescription without, and now looking back on it, like without any dietary advice, without any sort of real feeling that she'd been listened to, unfortunately. And that wasn't sort of the fault of the gastro physician at the time, it's just because we're not taught like these things at medical school. And so I'm hoping that, you know, lifestyle medicine becomes a thing. And in fact, I just got an email from my old university, Imperial. They're creating a new compulsory module called lifestyle medicine for year one and year two. So looking at the evidence base behind, you know, all these different holistic quote unquote interventions that actually have a massive impact on people. So hopefully, you know, we're training a new generation of doctors. And Bristol is pretty forward coming with this. I've lectured there a couple of times.
Dr Rabia: Oh right. Yeah, yeah.
Dr Rupy: They're amazing. They're really good.
Dr Rabia: It must have been that unconventional education.
Dr Rupy: Clearly, yeah. And Bristol itself is quite quirky. It's like, you know, loads of yoga events and all that kind of stuff. So...
Dr Rabia: It's pretty trendy.
Dr Rupy: Yeah. Okay. So we've just made your savoury oats. Let me get you a teaspoon because you can try that. It's a little bit hot, so...
Dr Rabia: Oh, so good.
Dr Rupy: Feel free to give me your honest opinion. Tell me what you think it needs, what, you know, whether tarragon was a bad idea, whether I need sage or oregano or something like that. So, yeah, please, please go ahead.
Dr Rabia: I'm in the habit of smelling. My husband always laughs at me. He's like, what are you doing? I'm like, mindfulness with food.
Dr Rupy: Are you a bit of a foodie as well?
Dr Rabia: I love food. Oh, yeah, right, yeah, massively.
Dr Rupy: We should chat about your favourite restaurants in London. I always love getting recommendations from people who are like, you know, really into food and stuff.
Dr Rabia: We're so not spoilt for choice. I mean, especially on a day like this. I mean, London is at its best in this weather. It's so good.
Dr Rupy: Yeah, totally. Yeah. Tons of rooftop bars I need to check out.
Dr Rabia: That is so intriguing.
Dr Rupy: It's unusual, hey?
Dr Rabia: That is so intriguing. Yeah. The textures work really well. Really well. And this could, I mean, this could make a good, like, as you say, it's brunch, so breakfast, lunch, like...
Dr Rupy: Do you ever accompany it with anything or?
Dr Rabia: I do. So usually, because the oats are quite soft, to bring a little bit of like a crunchy texture, I would serve it with some crushed hazelnuts that are toasted on top, just to give that little balance there. But, you know, you could do it if you didn't have a seed intolerance, then like some seeds, pumpkin seeds or sesame seeds, something like that. And then scrambled eggs, I would probably put through it or scrambled tofu if you're completely plant-based. So, yeah, that would work as a like a proper brunch dish. But it's, you've got to get over your sort of like a thought process behind porridge being a sweet dish and like, you know, with cinnamon and nutmeg and all those sort of flavours. So, yeah, so a little bit unusual, but...
Dr Rupy: So good. I'm so good.
Dr Rabia: And, you know, in the time that we were talking, so...
Dr Rupy: Yeah, yeah. Pretty straightforward. Very easy to make. So if you want to listen to the rest of the discussion that I'm having with Dr Rabia, tune into the Doctor's Kitchen podcast. You can find it on all podcast players and iTunes and on thedoctorskitchen.com. We'll see you there.
Dr Rupy: How was your lunch?
Dr Rabia: So good.
Dr Rupy: Or your brunch rather.
Dr Rabia: So tasty. Yeah, really good. Thank you.
Dr Rupy: We had it with a little bit of peach salad and some other spinach leaves and stuff. So it kind of hopefully was cooling.
Dr Rabia: It was. It definitely was. It was really good. Perfect for this weather.
Dr Rupy: Absolutely. So, let's talk about the brain-gut axis. This is something that is central to a lot of your research and I think it's one of those terms that's bandied around quite a bit without people really understanding what that means for them. So why don't we define exactly what we mean by the brain-gut axis?
Dr Rabia: Yeah, you're totally right. It's become a term that's quite trendy and yet, I don't think people have quite understood it to the extent that they can use it to change little bits about the way that they relate to their guts. So, put really simply, it's a conversation. So there's this conversation going on between the brain and the gut, right? So, and the conversation is going on on multiple levels. So what's occurring, let's say on the gut level, is that you've got the lining of the gut that is full of these cells and the cells are producing signals. So to use our analogy, the cells are kind of speaking. They are saying sentences, they're saying phrases. And these phrases are being communicated up to the brain. So on a really pragmatic level, we can understand that our gut is probably telling us when we're hungry or when we're full or when we need to go to the toilet. And those things are really quite simple messages communicated on, you know, a hormonal level. But what's interesting is the way that these are sent up to the brain is via the powerhouse of a nerve, a really long nerve, the longest nerve of the autonomic nervous system or I like to call it automatic nervous system of the body. You know, everything's occurring automatically.
Dr Rupy: Like breathing and homeostasis control.
Dr Rabia: Absolutely. And these signals are occurring like as fast as electricity along a telephone line, right? But for a long time, we thought that the vagus nerve, like any cell in the body, only understood nerve signals because it's a nerve cell, it's taking nerve signals. But it turns out it's multilingual. So it's kind of like Google Translate.
Dr Rupy: Yeah, yeah, yeah.
Dr Rabia: I'm loving these analogies. Yeah, like, I mean, this is how I explain it to patients because we need to kind of get it in our heads before we can work with it and move forward. And hopefully, you know, we'll do that. So, the cells are sending languages such as inflammation coming from immune cells or, for example, serotonin coming from our endocrine system, our hormone system. And a lot of people know that 80% of the serotonin is produced in the gut. Although, I will add here that not many people know that melatonin is produced by the gut as well. And you'll obviously been recommended, you know, foods, particularly foods that are melatonin containing. So that relates to the fact that sleep and the gut are related and all sorts of things. But the languages that are being spoken are inflammation by our immune system, hormones by our endocrine system, and also all sorts of other languages that the vagus nerve then communicates up to the brain to say, you know, this is what's going on down below. And then at the same time, and rapidly in a matter of seconds, the brain is then communicating back down to the gut in a kind of bidirectional conversation because we're talking about dialogue, like you and I, the two-way exchange of information, same as occurring. And the brain then tells the gut, okay, well, now's not a great time to go to the toilet because you're on a train or whatever. And I would really cite a book at this point called Gut by Julia Enders. Have you recommended that before?
Dr Rupy: Fantastic. Yeah, yeah. It's actually on my website as one of the recommended books for gut health. It's fantastic.
Dr Rabia: Perfect. It's so good. And it's probably one of the ones that I've come across that people most gel with.
Dr Rupy: It's very sort of pragmatic and it's very easy to understand. It's kind of simplified. In the very much the same way you're using a lot of analogies and stuff. I found patients really do find that useful.
Dr Rabia: Yeah. Yeah. And so I think she talks about, you know, in her in her second chapter, the relationship between the sphincters of the bottom. Do you remember that one? And it's it's like, honestly, even for me, I mean, I'm a gastroenterologist, I've trained in this for, you know, over 10 years, and yet, and yet, for me, there was a lot of information there. So it talks about, you know, the two sphincters, which are kind of like rubber bands around muscle groups at the bottom of the back passage and how one talks to the other and they're in this constant conversation. But the sensors in your back passage are constantly talking to the brain to say, okay, well, now's the time when you need to go to the loo and is it appropriate? And the sensors in the back passage are actually correlating with your past memory events, you know, to say, well, where am I? Am I with like a new partner that I've been with for like three weeks and therefore it's not really like acceptable to break wind or like, you know, what's where am I in this in this environment? So it's it's a mirroring between your internal environment and your external environment and that process is happening all the time. So I think what we've learned in the last like five, 10 years in this field in research is that the language is multilingual, that it's happening constantly and the dialogue works both ways. And I think those principles will allow us to remind ourselves as as patients, as people that we really influence, you know, the way we think about our gut influences the way our gut moves and the way it senses. And when we don't think good things about it and we don't form a good internal environment, then our guts develop problems like with with its function.
Dr Rupy: Exactly. And this sort of frames the discussion we're going to have about functional gut issues because if we're having so much of a bidirectional conversation with our gut and our brain, then there stands to reason there's a lot that we can do with how we think about our guts and what we do with regard to all these other sort of stress management techniques and um helping with functional gut issues. So why don't we dive into what we mean by a functional gut issue? Because again, that's something that's banned around a lot. I have a functional gut problem. And it's almost um it's almost like uh unintuitive to think of a functional gut problem being something that doesn't have uh a structural issue with it or a biochemical imbalance, but it's still manifesting in issues with sensation, motility, function. So what do we mean by functional gut disorder?
Dr Rabia: Well, exactly that. So, um, I have mentioned earlier that as a gastroenterologist, I put telescopes into people, right? So we call them endoscopes and we pop the telescope in and for me, it's useful to think about the gut as one long tube going straight from the from the mouth down to the bottom. And when we put a telescope into this tube, what we're seeing is just the inner lining. So we're seeing a layer of cells on the inner lining, a very important layer of cells, um containing lots of bacteria and viruses and fungi and all the rest of it. But nonetheless, a layer of cells. And we can use conventional scans like CT, MRI to look at the outside of the gut. So we can look inside and outside and we can say, okay, um if there is a break in the lining, um we can call that an ulcer. If there is redness, we call it inflammation. And what we see with the naked eye, we treat. We've got medications, pills, so forth for that. But there are so many more layers to this tube. So there are, if we peel back with our mind's eye one layer, you get a layer of connective tissue and within that nerve endings and within that immune cells. And, you know, the gut is called your second brain because it's got this nervous system made up of 100 million neurons that is functioning in and of its own, like another being. And so as we peel back the layers, all of these other processes are going on. And that stands to reason that some of those can also go wrong. And just because we haven't caught up with our testing investigations on how we examine the movement, the secretion and the sensitivity, doesn't mean it's not all going on. And so when those things malfunction, the function of the gut goes down. So we're talking, as you said, about the function of the gut. And what do I mean by that? Well, it's ability to contract and relax, so-called peristalsis, to move food along, and also its ability to absorb nutrients. So these are the functions of the gut as opposed to the structure, which is the long tube that can get red or scarred or whatever. And it's that arena that's going wrong for us because of our environment, our personality, our modern lifestyles, things have have got a lot of propensity to go wrong.
Dr Rupy: Absolutely. So that's what, what do you think is the reason behind why so much is going wrong with our guts at the moment? Because I'm inundated with tons of people in clinic and on social media asking about things to do with IBS or gut dysmotility or bloating or cramping and no, and everyone looking for a dietary sort of intervention for this. Obviously, my bias is food, the doctor's kitchen. But this is why I'm fascinated about the wider arena of lifestyle medicine because there's so much that can actually impact your gut. So why do you think we're seeing a lot more of these issues at the moment?
Dr Rabia: It's a really good question. Um, I would say that, um, there are, the answer is probably going to be threefold. So firstly, I think it comes down to modern lifestyle. Um, and within modern lifestyle, like you said, there are various components. One of which is diet, but there is, I mean, diet is undoubtedly one of the key players in this field, for sure. But for some reason, we've developed a bit of a preoccupation with identifying our food intolerances. And the reason why I think that speaks with what you, what the doctor's kitchen do is because effectively, some of the key messages coming out of your work is like, eat fresh, eat colourful. And all of those basic principles really do apply. But what's going on with patients is quite different. Instead of defaulting to those basic rules of life, we're looking at excluding certain food groups and we're ending up with irregular eating habits and a fear avoidance. You know, we go to a restaurant and we don't know if what we're going to eat is going to make us feel good or bad. And therefore, we end up with quite limited, I mean, I see our patients end up with really limited diets.
Dr Rupy: It's almost like you have that anxiety before you even start eating because you're worried about if this food is going to lead to issues in your gut. And you might even have like a hypersensitive hypersensitivity to a normal reaction that's happening in your gut where you have some fibre, for example, it causes a bit of bloating, but then you have that sort of anxiety compounding the effect of that.
Dr Rabia: Yes, absolutely. And that kind of goes back to what you and I were chatting about at the beginning, which is the idea that the way that we think influences our nerve cells and sensitivity. And therefore, a piece of food that not that wouldn't normally inflame or aggravate you mentally is going to. So, um, they always say, you know, you should eat in a really calm environment and not and avoid stress and, you know, stressful conversations around the dinner table because the very act of having a stressful conversation puts your adrenaline up. And adrenaline acts on the gut. It acts to activate the sympathetic nervous system, the fight-flight response, and you're ending up in a situation where you're telling your gut, actually, I've got a tiger in front of me and I'm in a situation to my primitive brain at least, which says I shouldn't really be eating right now. And therefore the gut's motility actually slows down and you become more sensitive. And so it's a no wonder that if you're having a really high-end conversation during dinner, that your gut starts to form patterns. And the patterns it forms then get replicated when you're not in a stressful situation, you know, and you're...
Dr Rupy: This is just reminding me of some of the stuff that my mum taught me when I was a kid, you know, if you're running around, you shouldn't be eating. If you're like, you know, shouting or you're not in a good environment at this point in time, you shouldn't be eating. All these sort of old wives' tales that have stood the test of time. There is actually a lot of science behind it.
Dr Rabia: She's going to be telling me like, you know, I told you so.
Dr Rupy: Yeah, she's going to be like, I took you this long to figure out what I told you in the first place.
Dr Rabia: So, so we jumped ahead a little bit. As we're going to be, we're going to be going all over the place. As is the function of the gut. Um, so functional gut disorders, what kind of functional gut disorders are we talking about here? IBS is the big one.
Dr Rupy: Yes. So IBS or irritable bowel syndrome is probably the most common. Um, and then you've got problems as we go back to that analogy of this tube going from the mouth all the way down to the bottom, you've got problems with reflux, indigestion, heartburn. Um, and what we would do is we put the word functional in front of that, which basically means that your telescope is normal and, you know, maybe even some other tests to examine movement and motility are normal. Um, so you've got functional reflux, indigestion, you've got functional dyspepsia, which is the medical term to describe discomfort in the upper abdomen, so above the belly button, and a sensation of feeling full too early or losing your appetite and bloating and so forth. And then if you move further down, you've got functional abdominal pain, which is just pain but without the change in bowel habit. And then you get towards kind of irritable bowel, which is probably the most common. So altered bowel habits, either constipation, diarrhea, or a mix.
Dr Rupy: And have you noticed, just on a personal level, over the last few years that you've been training in gastroenterology, that the acceptance of this being not purely psychological is sort of filtered down into the conventional thinking about how we approach functional disorders? Because when I was at medical school, initially, you know, we would sort of write off these people as this is all in your head or this is like a psychological issue. Go back to your GP, maybe start them on antidepressants, maybe see a psychiatrist. Do you think that's kind of changing now and the sort of the conventional mindset that this isn't just all in our head?
Dr Rabia: Yes, I think so. I think it comes down to, you know, everyone, I would say nowadays, and this is a credit to our profession, is having the conversation. So we are saying to patients now, most people, you know, what, how is your mood affected? What component is affected by your mood? And we know that, you know, having really bad symptoms leads to bad quality of life and therefore can cause mood symptoms, but also mood symptoms like anxiety and depression can then also cause gut issues. And this is the nature of the beast, the cyclical relationship. Um, so doctors are less dismissive of that. But sometimes patients find themselves not able to acknowledge on a conscious level that they have any anxiety or low mood. And that's okay, because not all of us do. But given what we know about the way the gut and brain are working, I think even if we can't acknowledge that we feel low, because maybe we don't, maybe we've got a very positive outlook, I think it's worth us considering that there are certain interventions that occur on a mind level, on a top-down approach that could actually benefit your gut. So I would really encourage people to not, I guess, depart from the stigma of thinking that they have to feel low in mood in order to have some psychology that will help their gut. Actually, psychology for the gut is needed anyway because of what we know about it.
Dr Rupy: And you know what? I find that a difficult conversation to have with patients sometimes because you don't want to insinuate that this is all in their head or that they do have a psychological issue that already has a lot of stigma around it. You do want to ask them quite sensitively about what are your current stresses throughout the day? Is it, you know, are you stressed at work? Does it have to be, you know, something that's very obvious or can it be, you know, the phone going off or a constant screens that we're attached to these days or, you know, the email sort of phenomena that has affected all of us in that we're expected to reply to them almost instantaneously. You know, are those the stresses that might be triggering gut disorders?
Dr Rabia: Yes, absolutely. Um, and before we go on to like talk more about the stress side of things, I just want to go back to your question earlier where you said, you know, why are we having so many functional issues? And I talked a little bit about, um, kind of environment, so the choices we're making surrounding food and so forth. But what's really interesting is that, um, you know, the microbiome, which is this bacteria colony of the gut, right? Like it outnumbers our genes by 150 to one. There's just so, you know, many organisms there. Um, this was formed, um, as well as your brain-gut interactions in the first three years of life. So between the ages of like birth and during birth and year three, a lot of these patterns were formed. Now, um, there's lots of factors that are associated with this, such as the mode of delivery. So whether you had a cesarean, born by cesarean section or vaginal delivery and the bacteria associated with that. Also whether you were breastfed or bottle-fed. But one of the factors that that really perked my interest is maternal stress. So maternal stress has a huge impact on their baby's gut bacteria. And I think as mothers, you think about what you put into your body during pregnancy, right? And you think about the supplements, you think about folic acid. But to what extent are we really protecting ourselves against stress? And the reason this is empowering is because on the one hand, you might think, oh, well, if my interactions and the patterns were formed at the age of three, then I clearly have no control over it. I don't think that's the case. I think actually we can use this knowledge to feel empowered because what it tells us is firstly that, you know, certainly we have no control over the way we're born. We can plan for it. But there's no way that the, I mean, the child certainly doesn't have any control, but mum doesn't have any either. She can plan for it, but it's out of her hands. So she can't choose to have a baby in a certain way and she can't choose to breastfeed necessarily. She can try, but all of these things are not entirely within her control. But what is within her control is her ability to say, okay, I am pregnant and I have a responsibility, you know, to think about the way I relate to my body now. So I think that's empowering and I also think it's empowering because I have a lot of patients who are amazing. They have toned their diet to an absolute key. They do physical exercise, they sleep well and they've got all the lifestyle factors sorted. And yet they come to me and they say, doc, I'm still feeling like I've still got a functional gut issue. What's going on? And I think one thing that is empowering is to say, to be honest, like, this is your Achilles heel. Like your digestive system is your body's way of kind of red flagging to say, you know, something's not right and it's if you're always going to have a bit of a predisposition there, a degree of acceptance goes a long way mentally, I think, to being able to progress and move forward to make changes.
Dr Rupy: I love the positive spin you put on that because I think a lot of people will look at that stress factor and be like, oh, I have no control of that because of the environmental stimuli and, you know, the fact that I have to go to work and I have financial pressure and all the rest of it. But the way you're talking about it is almost like this is in within your locus of control. This is something that you have a lot of impact on.
Dr Rabia: Absolutely. You know, I, I love the definition of stress that I got from my psychology A-level book. Like, can you believe after all our medical training? Like, you know when stuff just stands out in your head from like when you were younger. So the definition of stress from, and you may already like ascribe to this, from my psychology A-level was that stress occurs when there's a mismatch between the perceived demands of a situation and your perceived ability to cope with it. So a mismatch between the perceived keyword demands of a situation and your perceived ability to cope. And I...
Dr Rupy: That's so useful. Yeah, that's so useful because perceived is the sort of the key word there, isn't it? Because a lot of people can seem to have a lot of stressful things that they have to deal with, financial pressures, work, etc. But they still cope with it because they have great coping mechanisms, whether that be, you know, a good organized file or whether it whether they practice meditation or whether they have a supportive family. So, but then people who may have seemingly less stressful lives may perceive that to be more stressful for them. So it's again, it comes back to this personalized sort of individual approach.
Dr Rabia: Absolutely. Yeah. And I kind of, I mean, for me, this is just like, um, you know, hopefully helpful. Um, I imagine it like two scales, right? Like golden scales, or they could be any colour, just try and make it as regal as possible. Um, so on one side of the scale is like your the perceived demands and on the other side is your perceived ability to cope. And stress is the mismatch. So if you're in a stressful situation, ask yourself, what are the perceived demands and what is my perceived ability to cope? And can I reduce the perceived demand? Okay, maybe not. I mean, like, if you're in A&E, probably not. It's like if you're working a shift, I mean, the demand is high. But can I increase the perceived ability to cope? Because and what's interesting is this isn't just a psychological rhetoric. It's actually appearing in our studies. So when we look at the relationship between stress and digestion, the correlation is clear. No one can deny that. Even with patients who have a robust, strong constitution, you know, if you're preparing for a presentation, you get butterflies, you might need to rush to the loo and so forth. So the association, no one's going to be able to disprove it. But what we're not sure about in research, what's coming out is we're not clear whether it is a real difference in the body's ability to manage stress or whether it's the perception of stress that's the issue. So there was this study, I read recently, so it's St. Mark's Hospital in North London, 2004. And they looked at...
Dr Rupy: Just for the listeners, St. Mark's is one of like the world leading sort of centers for gastroenterology.
Dr Rabia: It is. Yeah, it is. Um, particularly in nutrition, yeah. Um, so St. Mark's did this study where they took IBS sufferers, so irritable bowel, and healthy controls. And they measured rectal blood flow. So the rectum is your back passage, it's the tail end. And they looked at blood flow as a surrogate marker of how the nervous system is functioning in that area. Um, there's obviously lots more nuances to the study, but just the basic principle I got from it was that they, they essentially had an intervention, which was psychological and physical stress. So we induced stress, and then we see what's the blood flow looking like, and also a lot of other parameters, how does your heart rate change, do you sweat more, so on and so forth. And what they found was between the two groups, the stress response was reasonably similar. But patients with IBS or a functional gut issue took longer to return to their baseline level than did healthy controls. So there was this lag time in the response. So we took longer to return. And the key thing that interests me so much, you can see how like passionate I am about this, because, you know, it's something that we did, they did in the lab and you say, okay, so what? So we took a little bit longer for our physiology to return to baseline. But actually that transcribes to a really important concept that I think is really empowering for people. And that is the concept of resilience. So resilience has been talked a bit about in the literature as well. And it's kind of defined as our ability to bounce back. So our ability to adjust and to cope with stresses or stressful triggers in our life. And so it turns out that our ability to cope with things and our ability to be resilient has a huge effect on our propensity to develop functional gut issues like IBS and sustain them.
Dr Rupy: Yeah, yeah. I can so, just going back to one of the, um, points that you made about the perception of stress versus your coping mechanisms. One of the anecdotes I found from one of my colleagues in A&E is a consultant in Northern Ireland. He presented at the flourishing in adversity conference, which is at the RCAM, the Royal College of Emergency Medicine, they do it once a year. And he's a really big fan of this concept of mindful snacking. So throughout the day, I mean, he's dealing with trauma cases, a whole bunch of like, you know, different external stimuli that are super stressful. Um, and every time he goes to wash his hands, he reminds himself of that being a mindful moment. So when I wash my hands, I'm going to breathe in, I'm going to breathe out, and that's going to be sort of my mindful snack. Or when I'm doing a cannula, I'm going to take everything out, I'm going to put everything on the on the, um, on the top of a trolley, I'm going to put my cannula here, I'm going to get my saline ready, I'm going to do that, and I'm going to have a mindful moment. I'm going to breathe in, breathe out. Uh, or when I'm doing suturing, it's like, I'm having a mindful moment. I'm just concentrating on the suturing. You know, there's these sorts of little points points in your day where you can actually improve your resilience to what's seemingly a very, very stressful external environment.
Dr Rabia: And do you think that that he would say that improved his resilience?
Dr Rupy: Absolutely, yeah. I mean, he's a, he's a mindfulness teacher now and he sort of talks about this with a lot of A&E trainees who obviously got a lot of stressful lifestyles and probably have a lot of functional gut disorders themselves. I don't think there's been any studies looking at that. But I think...
Dr Rabia: Yeah. Oh, brilliant. Yeah. I mean, yeah, I mean, look at what we do to ourselves in this process, in this system. I mean, you know, the system is fantastic, but I think we're not always the best at taking care of ourselves, are we?
Dr Rupy: It's the first thing I, one of the first chapters I wrote about in our book is that we're not pillars of health that people should look up to. We actually need to practice self-care before we start looking after other people. I mean, obviously, we're dealing with loads of other things, but...
Dr Rabia: You're completely right. Completely. I mean, um, the studies have been done in shift work as well a lot. You know, it's the disruption of shift work that I think, um, particularly in somewhere like A&E that disrupts digestive health. Um, so, yeah, a lot of studies have been done on that, I think, especially in nurses. So we don't necessarily have the system set up right for us yet. Um, but then again, I guess we're all working towards the same cause. So hopefully, hopefully there will be a sea change.
Dr Rupy: Yeah, yeah, I reckon so, yeah. And going back to your point about, um, pre-pregnancy nutrition and, uh, conception nutrition, because I just did a paper on it for my nutritional medicine masters and we talked about things like, uh, folate, definitely, folic acid, iodine, very important. A lot of people are thinking about that from a sort of neurodevelopmental point of view. We're actually quite low in terms of global sort of iodine measures. Um, uh, and people don't really think about where you get iodine from, you actually get it from like fish and dairy products and a whole bunch of other sources. Um, but I don't really talk about, uh, stress with my patients who are looking to get pregnant as well. And that is a very stressful sort of period in people's lives because they expect almost today with, you know, this instant gratification sort of, um, uh, acceptance that we should be instantly getting pregnant or things should happen to us immediately. That can compound a lot of stress as well that people have, particularly when they're trying to get pregnant. And as women, uh, you know, try and conceive later on in life, that can actually also put a lot of pressure on them as well. And that's something I haven't really talked too much about with regard to, you know, the process of getting pregnant and also the impact on on baby later on.
Dr Rabia: Yeah, and I mean, I guess I don't blame you because actually, like, the idea about stress, stress has taken a backseat. Like, the reason why, I always say, you know, people ask me like, why is gluten-free such a, like, is it a trend? Are people just going gluten-free because it's trendy? And I say, well, no, that's definitely not the whole picture. But the prevalence of celiac disease hasn't increased. It's still 1%. And therefore, the fact that like Pizza Express are doing, you know, gluten-free pizzas must mean that a large population are having an effect. And you will know be able to describe much better than me about the effects of gluten as a protein and so forth. But the point that I was trying to make in relation to what you're saying is that food is easy to manipulate, right? It's easy to go, I'm not, well, it's not easy. It's not, it's not like, it's easier, yeah. It's easier to go, I'm going to have a gluten-free roll instead of a normal white roll or whatever. Or I'm going to put this on my plate, I'm not going to put that on. And maybe we don't sustain the changes for very long and it kind of comes down to the idea of like, how do we form a habit, which is probably a whole another podcast in and of itself. But stress is harder to change and we don't necessarily think that we can do it. We don't feel empowered to because there's so much stress going on. I mean, how does one even live in the modern world without experiencing stress?
Dr Rupy: Yeah. And stress is quite like a big broad term as well. It's very an umbrella. It can, you know, incorporate a whole bunch of different things. You know, that sort of annoyance that you have when you look at something that the President of America has said, for example, or, you know, some sort of issue that you've had with a colleague at work. You know, stress can manifest in so many different ways that it's actually quite hard to pinpoint what we mean when we say the word stress.
Dr Rabia: Completely. And I think that's why that definition for me really helps me in my daily life. Um, because I mean, I'm definitely going to use that. Well, yeah, I mean, it just it came a long time ago, but I think the idea is that anything could be a form of stress, right? Low grade, high grade, um, you know, missing the bus can be a form of stress. So how do we take care of it, protect ourselves without becoming overwhelmed? Because there's no way of living a stress-free life. Like there's no, because we face demands every day when we wake up in the morning. But it's how do we process it? How do we perceive it? And things like mindfulness, meditation, yoga, breathing, it all, it all, it's about routine. Like having those things in your daily life so that you build up this protective piggy bank that you can reach into when you're really down and retrieve.
Dr Rupy: I can so, as you're saying all these analogies, I can so picture this in the clinic environment, like, you know, how you're explaining this to patients. So just to summarize, so we've talked about the brain-gut access, we've talked about how that relates to functional gut issues, we've talked about the concept of stress and what that means. And I love that definition. I'm definitely going to be using that. Um, how do we deal with stress now? Like what are the kind of stress-relieving techniques, the mind-body techniques, the mind-body interventions? It's something I talk about quite a bit in the latest book, um, in the lifestyle 360 section, where meditation is one of my, my favourite forms, but there's loads of different ways. So how do you, how do you get this across in clinic and what kind of practices that you do you talk about with patients?
Dr Rabia: Yeah, so I think it really depends how receptive people are. So it goes back to, you know, what we were saying earlier about our people, it's a spectrum, right? So firstly, you have to put yourself somewhere along a spectrum of, okay, do I have real anxiety and mood issues? If you're at that end of the spectrum, and I'm talking sort of high end, where you say, okay, my daily, I feel low, or I feel anxious, then that is something we need to address in the open. So we need to talk about it in a way that it is its own entity thing, it's affecting the gut, but really, I can trace that back to X, Y and Z in the past, certain traumatic events, maybe something in childhood and so forth. So for me, that's its own entity. So recognizing that as a clinician opens the door for me to referring to psychologists, cognitive behavioral therapy, and also certain antidepressants, which, as we know, work on the gut. So we use in our practice certain antidepressants like amitriptyline at very low doses. And patients are always surprised to be put on them for gut pain, but actually they are working synergistically, um, you know, at that level. So that's, that's one end of the spectrum. And then as you go sort of middle end of the spectrum, one of the things that I advocate, although it's not widely accessible, and hopefully I'd help one day to improve that, is gut-directed hypnotherapy. So there's a certain stigma attached to the idea of hypnotherapy.
Dr Rupy: Absolutely. Yeah. You just mentioned the word, like, what do you mean? Paul McKenna?
Dr Rabia: Right, exactly. Like, are you going to be put into some trance with a pendulum on a stage somewhere? And it's definitely not that. It's effectively, um, it was developed by Professor Peter Warwell, um, who's currently based in Manchester, and he, um, has developed this guided relaxation techniques that use metaphor related to the gut in order to allow the brain to reach a lower state of anxious functioning and therefore tap into some of the autonomic nervous system. So it goes back to not the fight-flight side of things, but the rest-digest side of things, where we are putting our nervous system into a relaxed state. And somehow this is what seems to help the gut. So putting the your nervous system, really tailoring down the frequency, putting it into a state where it can truly relax and truly rest seems to be the way that we are able to, um, access healing.
Dr Rupy: Yes, absolutely. And so we didn't talk about that actually. So the difference between the parasympathetic and the sympathetic system and how that's potentiated by different activities that we can do. So just broadly, what do we mean by those sort of different mechanisms, those sort of pathways?
Dr Rabia: Yeah, okay. So, um, we're talking about, um, here, the autonomic nervous system. So put really simply, it's automatic. Processes are occurring in the body, heart beating, um, breathing, which is under both conscious and unconscious control, um, and lots of other processes. And this is all happening automatically.
Dr Rupy: Which I believe is like purely by design, the fact that we can actually voluntarily and involuntarily have breath control. I think it's, yeah, it's a very powerful tool.
Dr Rabia: I can't wait to talk about that. But yeah, you're right. Like it's, it's, you know, the breath is our one of our ways to tap into that. And I say that like, you know, it's no evolutionary accident that the diaphragm is placed halfway between the gut and the brain. And we can manipulate that and the vagus nerve runs right through it. So, um, but to kind of uncover some of the jargon behind the automatic autonomic nervous system. So you've got, um, the sympathetic, um, and I also make this easier to understand, like that type of the nervous system is has sympathy.
Dr Rupy: Yeah, yeah, yeah.
Dr Rabia: For, um, my way of remembering it. So lame. Um, but it's like the sympathetic nervous system has sympathy for the fact that there are threats to our survival. And our primitive brain, our limbic system is kind of almost working against us in these modern times because there are no tigers and lions running around, but instead, tiny little stresses are appearing like threats. So what happens is is the sympathetic nervous system raises adrenaline and over a long period of time, cortisol, which is a different hormone related to stress. And we go into this kind of fight-flight mode. So heart rate increases, we start to sweat, blood pressure goes up and so on. Uh, pupils dilate and we are ready, we are ready to go. And then the other side of that, the flip side, again, going back to like golden scales, I suppose, is the parasympathetic. So it runs in opposition and what it does is it's it, um, allows digestion and rest to occur. So that is the side of us that enables us to digest. And it's like, you know, after we eat a big meal, we feel a bit lethargic. It's because our parasympathetic system is on the go. So our heart rate is lowered. And we can actually have the power to flip the switch, right? So we can take our foot off the pedal of the sympathetic, we can put it onto the parasympathetic, apply the brakes, and therefore allow the nervous system to seesaw between these two extremes to the benefit of our biology. So that's kind of how I would put it in a nutshell.
Dr Rupy: And so, let's talk about how we can actually dial up the parasympathetic system. So we're mentioning it briefly. I think we're dying to talk about breath work as one of those stress-relieving mechanisms, of which there are plenty of others. But I think breathing is particularly interesting from the evolutionary perspective, our design perspective. Um, what's been your experience of breath work thus far? And what do we mean by breathing as well?
Dr Rabia: Yeah. Apart from like, you know, the definition of it being a mechanical ventilation of the gaseous exchange service.
Dr Rupy: I love that.
Dr Rabia: Yeah. I remember that from A-level biology. You know, talking about mechanical ventilation of the gaseous exchange service. Yeah.
Dr Rupy: Oh, look at that. Can you believe how many, I mean, if we can do that right now in this moment, like trigger memories from our A-level, like the body is doing that all the time. Like there are these memories and these imprints and these patterns that are that happened back then during our A-levels that are still playing out now, like a video tape on repeat. And it's...
Dr Rabia: And I find those patterns of recognition can sort of manifest themselves when you're in certain environments. So like when I go to a large park, I automatically have amazing memories of being taken to parks when I was a kid and playing with my dad, for example. And that is a very stress-relieving activity for me. But for someone else, that might not be. That might be completely different. It might be, you know, triggering feelings of loneliness or being rejected by friends because they didn't play with them when they were four years old. You know, there's so many different ways in which people can manifest stress or relaxation in many ways.
Dr Rupy: Yeah. And we talked about, you know, like how, how do we, you know, because stress is, is going to be there, it's inevitable. But we could be, the first step is education and awareness, right? Which is what we're doing, like bringing the attention to the fact that there are these certain memory patterns and these footprints that exist in our life. And if we recognize the ones that are having negative effects on our body, we can change them probably, hopefully. So maybe the breath is one way to do that, maybe. Um, I think the challenge I've had as a researcher coming into this field is, you know, I, I mentioned earlier or I may have mentioned that I'm a yoga teacher. So for me, it was completely obvious that the breath is going to be the gateway to healing and relief. But then I got into research and I start to study this and I think, oh my goodness, I'm going to have to prove that like which breathing technique and how long do, what's the inhale to exhale ratio and is dysfunctional breathing the issue or is the asynchrony between diaphragm and chest breathing the problem? And so there's this whole endeavor.
Dr Rabia: The way you think about it from a research mindset, you know, how do we test this that, you know, this wasn't sham breathing versus actual, you know, something that's actually going on, but yeah.
Dr Rupy: Yeah, because surely the same is the case in diet. So it's like you know inherently, you talked about your mum earlier, she might have said, okay, turmeric is good for, I don't know, anti-inflammatory effect, for example. Okay, yeah, sure, that jumps on the trend and turmeric lattes are everywhere. But then as a clinician, what do you do with that? How do you, how do you justify writing that sentence, you know?
Dr Rabia: Absolutely. Yeah, because there's so many different things that can impact just that one addition to your diet. You know, is that turmeric in combination with a diet that is high in fiber or, you know, is it in a particular form of turmeric that's more bioavailable? Are we talking about fresh turmeric versus powdered? Is there a difference between the powdered one that's been sat on the shelf for two years versus the one that's just been made powdered by sun drying? You know, there's so many different things. And that's why this is just me going on a complete tangent here, but nutritional science is probably one of the most frustrating fields to be a part of because I find there's a lot of dogma and a lot of reliance on inaccurate studies or studies that are just fundamentally flawed from the get-go because there's so many variables that are confounding. And so they, they, they allow a multiple different ways in which to interpret the data. Um, but really what we need to be focusing on what are the principles and and what are the things that we can take away from from the studies that actually are translatable to clinical practice. And this again, I digress, but I find the most dogmatic people in nutrition are those that don't see patients because, you know, they'll be like, you know, low carb is the way or ketogenic is the way or we need to do this particular format of macronutrients. People don't eat macronutrients. People don't eat saturated fat in isolation. People eat food. And that's why, you know, when I was doing the research for both books and all the other stuff that I do online, I just found principles, as I do in clinic, is much better. You know, look at this plate, what does it look like? It's mostly veg, it's lots of different colours, it's good quality sources of fat that you find from extra virgin olive oil and seeds and nuts and stuff and fiber. And I find that almost the way I say it over and over again, I feel like people might be getting bored of it, but apparently not.
Dr Rabia: I'm certainly not. I could listen to you forever. Yeah.
Dr Rupy: Yeah, no.
Dr Rabia: Um, you know what though, this is exactly the mirror of what happens, you know, on the other things because, you know, diet is one aspect of lifestyle medicine, it's one of the pillars, as is other like physical activity and sleep and stress reduction. So when it comes to things like breathing, if we try and take ourselves too seriously and we do it in the lab and we try and nitpick and figure out, um, you know, in one way, it opens our mind to the various effects of it because what we don't want is to recommend a particular breathing technique that is limiting. So for example, one of the things that I've learned is that if you continue to breathe, okay, so what I should say is that, um, the inhale to exhale ratio of breathing is, um, is something that I have found validated. So the longer that you exhale, the the more you stimulate your vagus nerve and the more you stimulate the parasympathetic. So the kind of inhale for four, exhale for six has been found to be, um, the most, uh, tolerable ratio to breathe in for most people.
Dr Rupy: Okay.
Dr Rabia: Which is why it's employed so regularly in studies, um, you know, six cycles a minute, um, kind of thing. What we could do to increase the effect is breathe in for three, out for seven.
Dr Rupy: Okay.
Dr Rabia: But that's not that comfortable. And what it leads to is a little bit of hyperventilation. And therefore you get a little bit of, um, you know, a carbon dioxide release to in too large a degree. And that leads to other physiological changes. So you can go down the investigative route and it will lead you down a certain path. But what for me, I think the conclusion I've come to in the last sort of eight months is that breathing in the lab is very interesting, but actually in real life, there is no doubt that it has positive effects. And so we can take it only so far before we say, okay, let's be pragmatic. Let's go with principles. Rather than trying to prove that the four to six inhale ratio does X, Y and Z, let's just say that deep, slow breathing, so slow the frequency, take a deeper breath down into the diaphragm, that that has a positive effect. And that, you know, is an old wives' tale. I mean, you stub your toe, you take a deep breath, it relieves the pain. So can we be pragmatic with our research? Because that is sometimes what is lacking. Yeah, and pragmatism.
Dr Rupy: And so you were saying before that you've pivoted your research since, right? So you were involved in some studies looking at a particular type of breathing and the perception of pain. Yeah. Um, using a validated model, which I found fascinating. I don't know how you got it through ethics. But, um, you've since pivoted it, but would you mind talking about the studies that you did do and then how, you know, you might be, um, adding to that body of research and going down a slightly different path?
Dr Rabia: Yeah, I mean, so in terms of the breathing, the we're doing, so it's our lab that's done it. So for me, I started with looking at the literature review on breathing. And the reason I got into that was because of a particular product I'm developing, which we can mention later. So for me, it was always very driven to validate a product. Um, but the my lab itself, the Wingate, they're, um, it was a PhD student, um, Dr. Both, who did the study. And what he did was he looked at a healthy group of individuals and he instilled a what would be a pain response. So it was an acid infusion into the food pipe. And that stimulated the effects of what we would term as reflux. So increased acid and the effect that that has on the lining of the food pipe. And that instills a pain response. And then he would get people to deep breathe and there were very positive results to suggest that deep breathing lowers your threshold to pain associated with reflux.
Dr Rupy: What I found fascinating about it is, so, you know, you're introducing a painful stimuli that mimics what someone would have with dyspepsia or acid reflux. And you get, you controlled it with sham breathing or just, what was it just regular breathing or like...
Dr Rabia: Yes, so the sham breathing protocol is spontaneous breathing. So it's not, you count the breaths because the attention that you pay on the breath is a confounding factor.
Dr Rupy: Gotcha. Right.
Dr Rabia: So you count the breaths, it's spontaneous breathing, and then the, um, so sham versus, um, the intervention, which would be breathe for a certain number of frequency, which is inhale for four, exhale for six, and six breaths per minute.
Dr Rupy: And you found a significant difference between the perception of the painful stimuli that you introduced via the acid introduction to the the pipe.
Dr Rabia: Yes. So the lab, um, found that, yeah, exactly. So they, um, both and his team found that, um, there was a significant, significant difference.
Dr Rupy: So I find that fascinating. I know, I know. I want to see more studies that potentially replicate that finding. But you found that there might be some some issues with that or...
Dr Rabia: Yeah, so when I first, when I read this study, I arrived at the lab and Professor Aziz and I are quite keen to see if we can replicate some of this, but in the IBS cohort. So can breathing help to alleviate pain and anxiety associated with lower digestive issues, which is obviously slightly more complex because what we'd have to do is pop telescopes up people's bums, we would have to blow balloons up into the colon and then assess for whether the sensitivity of feeling that balloon improves. Um, so we were, we are, were looking to design certain studies that relate to that. And I think it's on the horizon. I think it's definitely possible. I think what I've recognized is that, um, the propensity to, I mean, the initial reflux study, which I described, was done in healthy subjects. So now what we're looking to do is try them in populations with functional gut issues. And I think that that is, um, going to be present its own challenges because, as we spoke about before, it's multifactorial. So whether or not the pain improves waits to be seen, but I'm certainly fascinated to find out.
Dr Rupy: Absolutely, yeah. And I think something that we were talking about a bit earlier that, you know, the issue with a lot of these studies, nutritional and interventions like breathing in isolation, is that it kind of negates to the obvious factor that it is so multimodal. Like there's so many factors that impact on someone's propensity to having IBS, for example, environmental stresses, psychological stresses, as well as what they're eating, as well as their sleep patterns and stuff. Um, how do we even begin to control that? I mean, I do that, you know, using the research out there, I will make suggestions on circadian rhythm disruption, sleeping at regular times, eating a certain way most of the time, if that if that's attainable for them, as well as, you know, exercise, movement, all these different things that have a plethora of effects on multiple different systems in the body. So that's why it's so hard to test this in a research environment. How does this translate to what you tell people in clinic and what do you think is the horizon on on lifestyle medicine interventions? So there's so many questions.
Dr Rabia: Yeah, I know. That's a big one. Okay. I couldn't agree with you more on that. I think the where we're faltering is that we are trying one thing at a time. Um, and of course, the difficulty is is in research, we like to see cause and effect. So how would one possibly try more than one thing and be able to with validity say that X leads to Y and prove causation? So I appreciate why we're having that approach in research. I think that's important. But for me, what's most pragmatic is, um, that that patients are so different. Everybody is so different that one thing to one person might be something to another. So there's what we call heterogeneity, so differences between individuals that need to be taken into account and also the individual's motivation. Um, and we, you know, don't spend enough time delving into that in order to provide what I would like to do eventually, which is a personalized medicine approach to each person. And a particular quote comes to mind that I also found really useful that I read recently and it really got me out of a low moment because I was going through these research thinking, I'm never going to be able to prove that that breathing in this particular way affects this particular thing. And then I thought, oh, well, you know, as you often feel, just scrap the whole thing. And this quote was from, it was from the journal Gut. So it's 2002 paper by a chap called Reed. And the quote came from a clinician, a physician who, um, was obviously reputed to have lived a couple of hundred years ago in Bath. And he is reputed to have said that it is more important to find out what kind of patient has the disease than it is to find out what kind of disease the patient has.
Dr Rupy: Fascinating. Yeah.
Dr Rabia: And for me, I don't know, something just struck a chord. I was like, yes. Absolutely. Yes. Like, and I don't blame us. I was saying earlier, we were we were chatting over lunch about the fact that our consultations are what, like 10 minutes? I mean, I get a 10-minute follow-up and maybe a 20-minute new if I'm lucky, which depends on the hospital I'm at. And I don't know how long you get in A&E, but, you know, how are you going to ask somebody about what kind of person they are? No time for that. And I don't blame us. But I think what I try to do at least is address the multimodal aspects, but in a way that's bite-sized and manageable. So I might try to identify, I often say to people, okay, you've got bloating, constipation, diarrhea, you've got loads of symptoms. If you could have one wish, and I take it really esoteric and they're like, who is this woman? I'm like, if you could have one wish, which one thing would you focus on? Because it's complex. And they say, okay, bloating. And I'm like, right, you need to look at the low FODMAP diet, but you also need to do some yoga. And just those two things. And you gauge the person in front of you and you say, okay, well, maybe you need to try this or try that. But one or two things usually does the trick. And in life, I would prefer someone to just feel better. Like, okay, yeah, like maybe, you know, we always say like, cut out gluten on its own, for example, um, to see if you feel better or then or cut out all of these things and then reintroduce. But I would just rather someone felt better. So if they're going to do a couple of things at the same time, maybe it's not scientific, but maybe they'll feel better.
Dr Rupy: I totally agree because in that sort of time-restricted consultation that we have as general practitioners and in A&E as well, you know, you want to try and hone in on what is the major factor when people come in with a whole bunch of issues, particularly if they've been waiting for weeks and weeks or maybe this is a chronic condition that's been going on over years. What is the next best step? That is always the thing. What is the next best thing that I can do or we can do together that's going to lead to a slow resolution of your problems. It may be one thing that actually leads to a whole bunch of improvements in a whole bunch of other things. But being listened to, I think is is fascinating. And I'm also fascinated in what your personalized medicine approach might look like in terms of a product. So tell us about that. I'd love to know a bit more about what you're working on.
Dr Rabia: Well, yeah, so I mean, anyone who's interested is so free to like kind of get in touch with me. Um, on my, I'm sure that my contact details will be available. So I think that's the goal. That's the kind of big, my kind of passion project. Um, in the meantime, in the last sort of eight months where I focused on the breathing side of things, I've been working on a government-funded project, which, um, looks at how do we merge art and science for the benefit of well-being to provide a well-being solution. So in the last couple of months, I've been working with artists to develop a prototype, which guides people in training in breathing techniques for the relief of pain and anxiety, um, using light-based biofeedback.
Dr Rupy: I've seen these. They look brilliant. They look so cool.
Dr Rabia: Hopefully. Yeah, I think I think it's coming along. It's really is coming along. And it's like essentially a mood lamp, um, that you can place in front of you. And, um, every time you breathe deeper based on a sensor that you have on a cushion on your back, the light shines brighter. And as you breathe with the diaphragm, the light will shine brighter and it will teach you to breathe deeper into the diaphragm to stimulate the vagus nerve with longer exhalation.
Dr Rupy: So you get like sensory and visual feedback almost. Oh, wow.
Dr Rabia: And then at the same time...
Dr Rupy: I need to invest in this project.
Dr Rabia: So bio-breathe. So, yeah, so it's breathing kind of better for your biology effectively.
Dr Rupy: Brilliant. I can't wait to see that.
Dr Rabia: And I've incorporated sort of the gut-directed hypnotherapy in it because it's kind of a stepping stone to for me to start providing patients and people with a more holistic approach. So the hypnotherapy is really key to alter the psychological processes and then the light is kind of an artistic element and so we'll see where it goes.
Dr Rupy: Brilliant.
Dr Rabia: Um, yeah, we'll see where that goes. And hopefully, I mean, I think diet has to come into it in some way because the people, I mean, you probably get this as well. People will say, oh, I can eat dairy one day and I feel fine and then I eat dairy another day and I don't feel fine. And it's like, oh, well, maybe there's something more going on than just the dairy.
Dr Rupy: Absolutely, yeah. Like, apart from me looking at, uh, time triggers, when you're eating certain things, which may come into the consultation depending on how much time we have. Uh, the environment, the surroundings, what you have with that food, for example, as well as your state of mind. I mean, there's so many different factors that it's very hard to get into one consultation where it may have an impact on your response to certain ingredients in your in your diet. And this is why I'm quite conscious of not getting people to restrict themselves as a first point of call, rather more understanding what are the other factors that can play a role in in someone's response. Yeah, which is very hard to do.
Dr Rabia: Very hard. Oh my god, we need some sort of tool to figure out, you know, where people are at, what is their biggest factor that influences them the most. And therefore, how can they work from that and then do the others later, rather than going maybe straight to diet or straight to breathing when they don't have, you know, they're not completely sure which one is the one that leads them, leads them astray the most. Um, so, and I think a lot of this will come from ancient philosophy. So like when you mentioned, you kind of alluded to food combining. So Ayurveda talks a lot about food combining. And I'm never sure whether I could put that to the test. I mean, is dairy with other groups of food like, you know, a different difficulty or not, like depending...
Dr Rupy: I'm just fascinated. I don't know how we're going to put that to the test.
Dr Rabia: I haven't actually looked into that as much as I'd like to, but, you know, Ayurveda is a recognized form of medicine in India. It sits alongside conventional therapies as well. And there's a lot of research that comes out of those institutions, but I just haven't had the time to look into it because nutritional medicine as on its own as a discipline is just so vast that that's even before we get into food combining, which I think is a whole other rabbit hole. But, you know, I suppose if we were to kind of condense what we've been chatting about today in a few words, it's lifestyle interventions in conjunction with, uh, you know, your, well, I suppose lifestyle interventions as a whole are so multimodal and can have an impact on multiple different systems in the body. And it's something we need to be a little bit more aware of rather than just looking at single interventions in isolation.
Dr Rupy: Yeah, absolutely. I think we need to begin to start having, um, you know, more conversations about how different things can influence us and prioritizing the ones that influence us the most. Not seeing, and also not seeing stress as the one that we can't manipulate because you can. Um, it's just about thinking, okay, how am I going to adopt mindfulness or meditation or breathing techniques, for example? Which, how am I going to ensure that my nervous system is put into a state of rest frequently, especially when I'm eating? Um, but at other times as well, because sleep is not, sometimes, I mean, you wake up and you don't feel rested. And I think that's a reminder that you need to put your body into rest at other times of the day. Um, so that's an area, um, and it's just using all of those things in tandem, figuring out, looking at the person you are, figuring out what are my resilience levels, how do I manage stress, how do I face this, and then employing that for the benefit of of you, I guess, is is what we've talked about roughly. And loads of other things along the way.
Dr Rupy: Well, I hope you thoroughly enjoyed that podcast with Dr. Rabia. She is absolutely incredible. I love her research and I love her ethos as well. And the fact that she's a yoga teacher, she's combining conventional medicine, she sees patients weekly. You know, it's a breath of fresh air. To summarize what we talked about, the way we think impacts the way we digest and vice versa. A complex model of health requires a complex call to action. So it can't just be about breathing, it can't just be about diet. It has to be looking at the lifestyle intervention tools that we have at our disposable. So that includes a diet that is colourful, largely plant-based, lots of different fiber sources, as well as stress-relieving techniques that can include breathing, but can also include walks in the park, meditation, yoga, different forms of exercise. And exercise itself could be one of those interventions that improves functional gut issues. Diversifying our diet by focusing on lifestyle interventions and taking the pressure off food intolerances as the only answer is a way of improving gut health. We talked about autonomic nervous system dysfunction that has been implicated in visceral hypersensitivity, so the sensitivity of our guts that leads to symptoms. And deep breathing may be a way of increasing parasympathetic nervous system tone, so it increases that rest and digest, and that can improve chronic visceral pain syndromes, a fancy way of saying IBS and other functional gut problems. There is a lot of evidence for stress reduction techniques and improvement of gut issues that may not have a physical cause. And this is something that we've talked about on previous episodes looking at inflammatory bowel disease and stress for type two diabetes. There is a need for multimodal changes, the complex interplay of lifestyle changes are more technical than you think. So simple things like breath work, stress reduction techniques, dietary change, impact a whole host of pathways that can improve and protect ourselves against a multitude of diseases, one of which is functional gut problems. I highly recommend you check out Dr. Rabia's website. It's on thedoctorskitchen.com. Biobreathe is the project that she's working on. Please, please, do go and support it. You can find all of this information and more at thedoctorskitchen.com. Subscribe to the newsletter for weekly science-based recipes, content and much more to help you live the healthiest, happiest life. Give us a five-star rating if you like this pod. It really does help spread the love and the message. Tweet us at @doctors_kitchen. Check out the Instagram, YouTube, and of course, don't forget to order a copy of the latest book, Eat to Beat Illness. A whole bunch of research posted on this podcast is at thedoctorskitchen.com as well. Have a fantastic day and we will see you on the podcast next time.