Ben Brown: You know, it's like the demonization of a process, like inflammation is a similar story, right? It's like a bit of inflammation is good, it's totally normal, happening all the time. Same with your gut. So, you know, this whole fixation on leaky gut is needs to be treated with a degree of caution and it probably needs to be defined and contextualised as a problem before you start worrying about it.
Dr Rupy: Ben, so lovely to have you back on the podcast. I think we're going to talk about therapeutic diets today, but more generally, what are the foods that boost and repair the body, reduce inflammation and by nature are anti-aging?
Ben Brown: Yeah, it's a big question. There's a lot of different foods across the spectrum of what we eat that contribute to anti-aging in the sense that they optimise health and help prevent age related chronic disease and you can break it down into like food groups, you know, at a top level and then get into specifics. But at food groups, it's really clearly, you know, fruits and vegetables, but specific categories within that that in particular are really rich in nutrients that support metabolism and optimise function. And the real key standouts are things like the green leafy vegetables and berries and things that are really rich in polyphenols and phytonutrients as a starting point.
Dr Rupy: Yeah. Yeah, yeah. We just did some work on berries actually, doing a deep dive into the benefits to brain health, cardiovascular health, even blood sugar as well. It's actually some really interesting interventional studies as well as observational data looking at the benefits of of just getting berries in every day.
Ben Brown: Yeah, absolutely. You're you're 100% right and it's, you know, there's sort of levels of data that point to these foods. Like you say, the observational studies and then there is a surprising amount of interventional stuff, especially on berries, you know, and the effects are really striking, like in terms of optimising metabolism, blood sugar regulation, cardiovascular health and one area I find really interesting is like cognitive function as a biomarker of like brain aging, right? And and there was a great researcher, she's unfortunately passed away now that Martha Morris who pioneered what they call the MIND diet, MIND. Which is a version of the Mediterranean diet that's been optimised for brain health and it was actually her work that really isolated in a sense the benefit of these particular foods, the green leafy vegetables weren't so much on the radar before her work and they they actually developed a metric for looking at how much these foods can shave off your brain aging, basically, like years. And when you look at the green leafy vegetables, it's like nothing comes close. And then a bit behind that's the berries and then it's things like nuts, you know, walnuts in particular, almonds, things like that and yeah, so like thanks to that sort of work, we've got a good idea on what's particularly good for you.
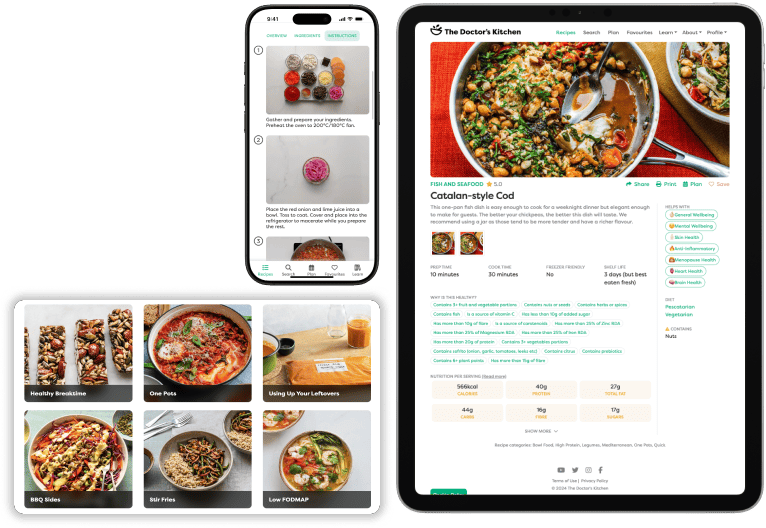
Dr Rupy: Yeah, it's amazing, isn't it? Because I think a lot of people are looking at cool and sexy additions to their diet like adaptogens and specific types of drinks. And we have this thing in the Doctor's Kitchen, just get your daily BBGs, beans, berries, greens and seeds and nuts.
Ben Brown: Perfect. Yeah, yeah, yeah.
Dr Rupy: If you get your BBGs in, you're good.
Ben Brown: Yeah, and that's the thing, like and this is the one one of the things that infuriates me as someone who works in this field is is all this hype around like super foods and I'm like, hang on a second, there's so many cheap, accessible, local super foods that aren't being hyped that you need to know about, right? And BBGs is a great way to do that.
Dr Rupy: Yeah, totally. So we're going to talk about therapeutic diets, right, for gut health. Um, I think, uh, you did this wonderful presentation at your nutritional medicine conference that you hold every year. Um, but I I guess before we dive into specific therapeutic diets, why don't we talk about gut disorders and specifically which diets have perhaps the most evidence, uh, for for for use in gut disorders?
Ben Brown: Yeah, absolutely. So I think a good place to wind it back is to define what we're talking about and you know, gut disorders mean a lot of different things to a lot of different people, but like medically you can break these into categories and one of the most common ones is something we call IBS, which you know, isn't a very helpful term, but what it's defined by is like pain, bloating, discomfort, changes in bowel habits and I think an important thing for people to understand is that this can be really severe for some people. It can really impact their quality of life, daily function and be hugely problematic, leading to things like anxiety, fatigue and so forth. So they're not, you know, we're not just talking about a little bit of bloating here. It's something that can be quite impactful in people's lives and and that is is a broad category that and and this is one of my things with with gut disorders is is um, it can be broken down into different areas. Although we've got this general category, there are there are almost like subtypes of IBS that we need to be talking about, especially in relationship to what diets work because there are different causes for the same set of symptoms. And this is one of the problems is is that this is often overlooked. It's like, you know, you have these symptoms, you're, you know, you have other serious problems ruled out medically and then you're sort of lumped with this diagnosis and and you're told, maybe take a probiotic, try and eat better and and and there's not a lot of solutions.
Dr Rupy: And actually anyone listening to this with they're a medical professional like a general practitioner or a patient, probably recognizes that chain of events very well. You know, so you go in, you have these really debilitating symptoms and in a lot of cases, you know, I think most people have come to understand IBS as bloating like related symptoms, but there are lots of different uh uh uh symptoms related to irritable bowel. And then you go through all these barrage of investigations and in some cases as severe as having an endoscopy as well as bloods and everything else. And then everything's quote unquote normal, in which case you're carted back to your general practitioner and then there's not really much else. So this is sort of the lay of the land, but yeah.
Ben Brown: Yeah, exactly. And it's not controversial. Like you say, everyone knows this from the gastroenterologist to the doctor, to the dietitian, to the the patient. It's it's a common experience and speaking to this, I I um, had a paper published in the journal gastrointestinal disorders with a provocative title that was does IBS exist?
Dr Rupy: I wanted to talk to you about this. Yeah, yeah, yeah. It was a great title.
Ben Brown: We're heading there. And um, that title helped actually, it got that paper a lot of traction because it was intentionally trying to stir things up a bit. And the whole premise is is that actually there are things that we're often overlooking within the workup or or I should say assessment of IBS that we could be doing that we're not currently that can identify underlying causes that have diet and lifestyle related solutions or not necessarily solution, but things that we can be doing to support symptom reduction and management. You know, so, so I think this is a huge area that you know, is coming out of the woodwork around better management and better support for people who are suffering from digestive symptoms.
Dr Rupy: Yeah, yeah, yeah. And and looking a little bit further into the various subtypes of IBS, can we qualify some of them for folks at home? Like what are the predominant symptoms of different subtypes of IBS?
Ben Brown: Yeah, absolutely. So there are the way I see it is there are like two sets of subtypes. There's the traditional ones that that, you know, everyone working in this field will know about. Um, so this is diarrhea predominant, constipation dominant, like mixed type, which is a bit of both and then they're like might be pain, there's a few different versions of it.
Dr Rupy: Pretty broad, aren't they?
Ben Brown: They are. Yeah, yeah, yeah. And and they're a little bit useless in that often people who have constipation will alternate with diarrhea and will get pain and and it will change and you know, so you need to be careful with these classifications because they're dynamic. And the other and this sort of comes back to some of the work that I've done is is that I think there are subtypes based on identifiable um, contributing factors to people's symptoms. So, you know, an example of this might be, you know, we we have some emerging research that suggests that um, nickel in the diet, which is a metal, um, could be contributing to symptoms for some people. So the way I see it is is this is potentially a subtype of IBS is you have like a nickel sensitive subtype. And this is one that's definitely being overlooked for good reason. It's very new work that's being done in this area, but it's really important and and there are reoccurring things around this. It's like, you know, it could be this or it could be a food sensitivity of some sort and so on and so on.
Dr Rupy: Yeah. Yeah. And and in terms of um, uh, the traditional diets that are used for IBS, what why don't we go through some of the the general approaches that people have when they they have either a specific subtype of of IBS or a other symptoms.
Ben Brown: Yeah, absolutely. So there's like currently within the within the UK, you sort of conventional management of IBS, there are two main dietary approaches that are utilised. The first is what we call a BDA or NICE guideline diet. Um, it's also sometimes referred to as a traditional IBS diet or a traditional diet. And to define that, essentially what it means and what the approach involves is um, some really simple practical things that people can do that we think are very likely for most people to help reduce symptoms. So that is like, you know, regular meals, eating healthier, avoiding things that can cause excessive gas, like excessive intake of onions and beans and and so on. And um, you know, excessive alcohol, these kinds of things. They're fairly simple, logical, easy to apply things. And that approach has really good evidence behind it. It works very well and um, is a really is generally recommended as the starting point. So if you have symptoms and you're thinking of embarking on a diet, this is where you want to start because it's easy, accessible, it's not going to change your diet too much and it might work. There's a high likelihood. So before you get into some crazy, you know, extreme diet, start here. And then the next tier in, you know, in the conventional management is is what we call the low FODMAP diet, right? And that's a lot more involved. So it really requires care and assessment with a nutrition professional like a dietitian and uh careful management uh through the dietary process. I mean, you can do it yourself. There's lots of DIY versions and you know, self management's not necessarily a bad thing, but good to have care and advice because it is quite restrictive and it's, you know, important to be coached through that. And that diet basically involves um, restricting certain types of carbohydrates that are easily fermented by gut bacteria and produce gas. And it's not that the FODMAPs just cause gas, it's that the gas actually has other effects other than just causing farting. It actually aggravates like the the nervous system and it can contribute to a lot of the symptoms we see like constipation, but also diarrhea and also pain and also the feeling of like distension and bloating and and so on. So and probably other things like it, you know, it like even mood and fatigue might be affected.
Dr Rupy: I was going to ask you about that because there's this term that I've come across after chatting to another podcast guest, Monty Lyman, who's written a book all about the immune mind and how our microbes and our mind and our um, uh, immune system are intimately linked as as you well know. And he describes something that he suffered with, which was an irritable bowel, which led to an irritable mind as well. And so this connection, you know, with not just traditional digestive symptoms of constipation, bloating, diarrhea, or alternation between the three, but also mental health symptoms that perhaps might go undiagnosed or or not picked up on as being related to an irritable bowel issue, um, unless you had a practitioner that was holistic minded.
Ben Brown: Yeah, exactly. And I mean, this is the, you know, you well know is like one of the great conundrums in medicine really is that it's difficult to compartmentalise things and ignore other areas of the body because it's all interconnected. So it, you know, you frequently, you know, in medicine we call that a comorbidity, which is a silly term in the sense because it's really it's just the person, you know, and it, you know, it sounds wishy washy, but I think we need to get back to like holistic medicine as a term and start thinking about how everything interconnects and the whole body and the whole person and you know, it's because that is what happens. Like it's we know in IBS, there's frequent comorbidities of anxiety and stress and sleeplessness and depression and so forth. And we also know that it's not just because you've got horrible symptoms, it's because there's a biological relationship between the two and you know, thing there are ways we can explain that biologically like the gut brain axis or the effect of certain foods that could be aggravating both areas, like your your mental health and your gut health could be affected by the foods that you're eating and so on and so on.
Dr Rupy: Yeah, yeah. Before we go into the FODMAP in a bit more detail, I wanted to ask if you had an idea, like a ballpark idea of uh, how effective the traditional diet or like a NICE or BDA uh, standard diet is for IBS symptoms?
Ben Brown: Yeah, it's a good question and I I don't know. It it seems to um, have a like a statistically significant effect when you look at it in in the research and generally it appears to be quite comparable in effectiveness to the low FODMAP diet. So there have been quite a few head-to-head studies and um, the efficacy seems similar. And that I can speak to is the low FODMAP diet has like a, you know, and you know, they say 80% of statistics are made up on the spot. But but it's about like, you know, there's a really good response rate, but it's about um, 70% or so. So there's like one in four people roughly that don't respond very well to a low FODMAP diet, which I think is really interesting and we can come back to that because it opens up that question like why aren't they responding, but um, yeah, the the take home is is that there's a reasonable chance that you are going to respond and you'll get a a decent symptom reduction from a less extreme diet that isn't going to be, you know, putting you potentially at risk of, you know, not getting a diversity of different ingredients.
Dr Rupy: You actually had this amazing uh, slide from um, uh, a journal of gastroenterology and hepatology that we'll put put on the screen for folks on on YouTube. But there was this uh, head-to-head comparison of traditional diets versus um, low FODMAP diet and a gluten-free diet. And I thought that was really impactful when I saw that on the screen when you when you had up on your presentation, just to show the comparable efficacy of something. But what isn't demonstrated in that is just how restrictive one is versus the other. And so you want to go for the sort of like um, uh, the the lowest barrier before you start going to, you know, more hurdles.
Ben Brown: Yeah, for sure. And I think I love these kinds of studies, like comparative studies because you're comparing possible interventions against each other and looking at things like efficacy, but also and you you really astutely point out is is like the real world things that matter. Like it's not only about efficacy, it's also about acceptance with the patient and the ease ability of implementing it. And this study was a brilliant example is is, you know, there there was almost comparable efficacy, but the traditional diet was way more acceptable because it's so much easier to do. And and they've been other examples where they compare head-to-head like a gluten-free diet versus a low FODMAP diet versus a Mediterranean diet, you know, which do you think wins? Well, efficacy, they're all similar, but people love the Mediterranean diet and we're much more likely to stick to it because it's way better. Like you get to it's like about abundance and inclusion rather than exclusion of foods, right? So it's like a very different way of approaching things and it just makes sense.
Dr Rupy: Totally. Yeah. And you you described the FODMAP diet as something that basically went viral when it kind of came out. Because it was, I remember first coming about coming across it, I think I may have been in Australia and it came out of Monash University, I believe. And it just got widely popular really, really quick. But I I guess maybe before we talk about the FODMAP in a bit more detail, what is exactly a FODMAP uh, for folks at home?
Ben Brown: Yeah, so this is where it gets, it's, you know, confusing, so you'll have to roll with this, but basically FODMAP is an acronym for different types of starches and sugars. So it's fermentable oligo, di, mono, something, something. You don't need to know basically, but essentially what the diet is is the whole premise of the diet is you're trying to work out which of these um, the individual is reacting to and which you need to reduce or exclude um, to to reduce symptoms basically. Um, so that's essentially the premise of it and as you rightly point out is that it it this particular dietary approach has gained a lot of traction over the years. So there've been a lot of human clinical studies. It's been built into management guidelines and and so forth. So in a, you know, in the world of science and medicine, it did go viral. And I think, you know, the the relevance of that like term applied to a medical intervention or, you know, nutritional medical intervention is is that maybe there is a bit of hype that we need to be questioning around it. Maybe it is like a viral phenomena and we should be thinking about that in the sense that there might be other approaches or other ways of thinking about things that are not necessarily only a FODMAP diet that's important.
Dr Rupy: And you you we alluded to this a bit earlier, but you know, um, only a third of people tend to respond to a low FODMAP diet, which is quite exclusionary in itself. What what are your thoughts as to other things or other exposures that could be leading to IBS symptoms?
Ben Brown: Yeah, so I think like winding it right back is when you have gut symptoms or IBS, which are really interchangeable in some sense, is that you need to think, well, well actually it's like um, there can be a lot of different causes basically and we know this, it's not controversial. It's what we call like a heterogeneous disorder, meaning that there are a lot of potential things that are aggravating symptoms for people and the biology of it, like what's going on in your body and and things like your microbiome and your metabolism related to that illness are really different from person to person as well. So it makes sense then that there's not going to be a single solution. Like it's it's just not going to happen. Unfortunately, be great if it did, but it doesn't. And so with interventions, whether it's a medicine or lifestyle changes or dietary changes or a magic probiotic or something like that, it's not going to work for everyone. You know, some people will respond because it fits what's going on for them. But the you know, the real trick is like working out what is going to benefit an individual um, and and what is less likely to be useful. And and that's the big challenge at the moment in medicine in general, you know, is is really getting better at personalization. And you know, so that's the big picture. But then the the answer to the question is like what are some of the other things is, you know, there there are a lot and you know, I I sort of divided into into three general groups. One of them is nutritional things that could be contributing to symptoms. One of them is like lifestyle things and the other one is like what we might call more like functional or or um, metabolic things, like things that are happening in our physiology that could be um, that could help explain why we have symptoms. So it's sort of wind it back to those three and the nutritional piece we can dive into, but it's like there's quite a lot of different foods that could be aggravating symptoms and there's also a lot of conversely therapeutic approaches that are very different that could help people. Again, trick is knowing who and and same with lifestyle, it's like there are lots of different things, but the big ones are like regular exercise. Sounds too simple, but it has a huge impact. Yeah. Uh, sleep and circadian rhythm is the other one and stress management, like they're the big ones that are that are really important. And then um, in terms of the, you know, the the more intangible sort of functional things for people, it's like that probably in most cases is going to require some testing. So it's like things that are going on that we need to be looking for like, I don't know, um, you know, one example is um, you know, an issue related to your pancreas that can be affecting enzyme output that could be contributing to symptoms or it could be like changes in your gut flora that are contributing to symptoms in a specific way that we might be able to investigate or or you know. So there's there's several examples like that, but that's the sort of thing I'm talking about.
Dr Rupy: Yeah, absolutely. And I think anecdotally, I know that people tend to gravitate to the more sort of like um, uh, uh, sexy for one of a better word, uh, investigation led approaches to figuring out their symptoms before doing the basic stuff. And actually something that spoke to what you were just discussing just just mentioning here about lifestyle was the comparison of low FODMAP diets versus uh, yoga. There was a paper that you you brought up with that and it showed it was as efficacious. Am I saying that?
Ben Brown: Yeah, I love that. Like that was like for me that was just like these sorts of things just open up a some like serious questions I think is like, you know, if you if, you know, this study just for listeners is like you have a head-to-head comparison of a dietary intervention versus yoga, right? And they worked equally effectively. So for me that, I don't know, maybe I'm overthinking it, but for me that opens up like some serious questions like, you know, which is the better intervention firstly, like for for patients, if maybe we should be giving them the option before you make radical changes to your diet. Do you want to try yoga? And then the other big one that is for me is even more interesting is is like, how is yoga working? Like what's going on there? Does it mean that when you do yoga, you enhance your tolerance to dietary FODMAPs? Like so can you skip the diet and improve tolerance to food by doing something like yoga? And it's not a crazy question because there are examples of interventions that do seem to be doing this is like they're actually enhancing your tolerance to your diet. So these sensitivities uh, you know, fall into the background and these elimination diets become less necessary. Which is cool.
Dr Rupy: Yeah. That's that's a really interesting thing about herbal medicine in general is that because you're using the entourage effect of these whole plants or derivatives of plants, you don't really know whether it's the antimicrobial action, the anti-inflammatory action, the sort of like anti-motility action that could also be helping with the constipation that's leading to. So there's all these different things that are going on. And I think on the wider question of like uh, experimenting with these antimicrobial herbs versus antibiotics, it's probably the one playground that I think is relatively safe because, you know, you wouldn't want to try herbal uh, recommendations for a chest infection, let's say, that could spiral out of control into full-blown sepsis and lead to someone going to the ICU. At least with SIBO, you know that, okay, if you try something and it doesn't work, it's not going to lead to like a case like sepsis, which is, you know, going to obviously have potentially uh, life-threatening outcomes.
Ben Brown: Yeah, absolutely. It's a really good way to put it and you know, when you're when you're dealing with something like, you know, trying to relieve gut symptoms, there's not a lot of harm in trying it. Um, I mean, theoretically, it could be disrupting your microbiome like an antibiotic does. So long term, you want to be careful with it, but a course and maybe two courses, um, is not a lot of, you know, risk.
Dr Rupy: Yeah. Yeah. I don't think I I haven't come across anything that, you know, like um, uh, C diff related uh, cases with antimicrobial. Would would did Jerry's group uh, publish what what herbs they use? Was it was it?
Ben Brown: They did. Yeah, so they used um, about four different products. Um, they're all US based, unfortunately, but they're very much like the kind of products that we use here. And their approach is really interesting is they cycle it. So the way they do it is is if you, you know, if you get a positive breath test and and the symptoms fit and they think it's appropriate, they try a four week course. And then if that product doesn't work, they switch products, try another course and see if you respond to that and and then they stop. Um, so it's I think it's a really good pragmatic approach and and makes sense and you know, it's also reassuring to know the kind of products they use is like, you know, a lot of the formulas that are out there.
Dr Rupy: Yeah. Yeah.