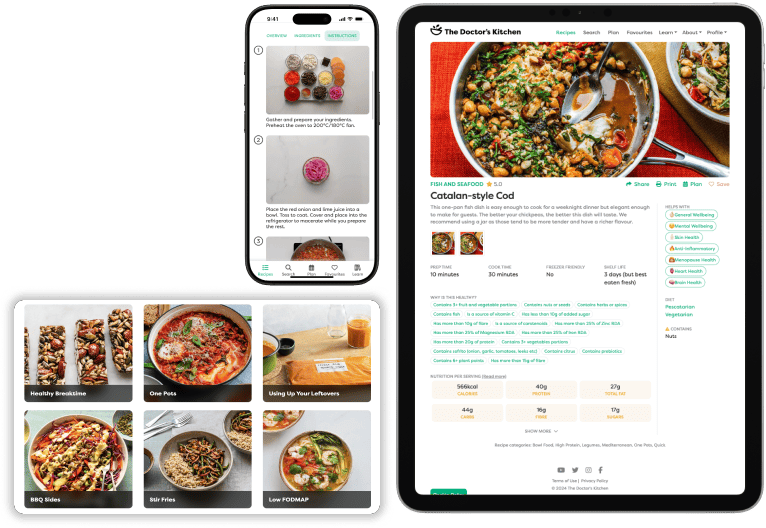
Dr Rupy: Can when you eat be as important as what you eat? Well, my next guest definitely thinks so and has spent his entire academic career studying the effects of circadian rhythm on everything from heart disease, exercise capacity, cognitive health and yes, diabetes. Satchin Panda, PhD, is a professor at the Salk Institute in La Jolla, California. His lab studies how circadian rhythm in metabolism is an integral part of metabolic health and longevity. In preclinical animal models, he discovered that consuming all calories within a consistent eight to twelve hours, also known as time-restricted feeding, can sustain daily rhythms. And one of the commonest topics I'm asked about is whether time-restricted eating or eating within rigid windows is advisable. And so I was fortunate to spend some time with Dr. Panda himself today, whose research I've been privy to for many years. And studies have shown that this practical tool can prevent or even reverse chronic diseases and increase lifespan. And today, you're going to learn a lot of things. What circadian rhythms are, the biggest drivers to rhythm, eating, light and exercise, eating strategies for shift workers. And actually, why technically, according to the definition of what a shift worker is, more of us are actually shift workers and not just firefighters and medics. And also how we separate the effect of time-restricted eating from the inevitable calorie deficit that can sometimes confound the results. And we also talk about the benefits of intermittent fasting to insulin release, your gut, inflammation and fat breakdown. You're going to find out so many elements of time-restricted eating in today's episode. I'm sure there are going to be lots of follow-up questions and we'll probably have to do another episode on time-restricted eating. But if you are interested in more of this, we've done an episode with Dr. Walter Longo that you can find in the podcast library as well. You can find Satchin's book, The Circadian Diabetes Code, in all good bookstores and the links to which are all on the doctorskitchen.com. And whilst you're there, you can download the Doctor's Kitchen app for free and there's a 14-day free trial from the App Store. And whilst you're on the doctorskitchen.com, do check out our newsletter, Eat, Listen, Read. Every week, I send you a recipe to eat, something to listen to, something to read that will inspire you to live a healthier, happier week. That is our weekly well-being newsletter and lots of you are absolutely loving it. For now, on to the podcast. This is my conversation with Dr. Panda. So Satchin, look, it's a pleasure to have you on. Love the book, love the previous book. I've been following your work for a while now. I've heard you on a whole bunch of podcasts, but the things that I haven't heard about are a bit more about you. So where you grew up, what you were doing when you were a teenager. Where were you born?
Dr Satchin Panda: I was born in a province called Odisha in India. It's on the east coast. Gets a lot of plenty of rainfall and the primary economy when I was growing up was agriculture. So that's how I grew up. And I think in my book I mentioned I mostly grew up next to my maternal grandfather who used to work for the Indian railway and do night shift work sometimes. And I was feeling like, wow, he's a superhero because he could stay awake throughout the night, do the work and daytime he could still play with me. And what I didn't realise was that was putting a heavy toll on his health. And just after he retired, he got diagnosed with Alzheimer's and passed away pretty early in the in his 70s, early 70s. Whereas my paternal grandfather lived a little farther on a farm. He did not have, I still remember there was no electricity or running water in the village. And he was a farmer. He used to grow almost everything from his from the land, except he used to buy only salt and sugar from outside. And he had no access to any modern healthcare, but lived in sync with his, I would say, circadian rhythm because no electricity for a long time. And he lived to the age of 93.
Dr Rupy: Wow. Wow. That's amazing.
Dr Satchin Panda: So I think that was a great experience to see the contrast. Of course, I didn't relate any of that to circadian rhythm at that time, but now I can.
Dr Rupy: Yeah, of course. Yeah. It's interesting, isn't it? You you look back at the the arc of someone's life through the lens of our experiences today and looking at the science and you can sort of piece together the dots of, okay, why were they able to last so long or live for an extended period of time beyond the life expectancy without the modern healthcare essentially, without access to modern drugs or interventions. It's it's pretty fascinating. And what about your your own childhood? So when did you when did you go to school and when when did you actually decide that you wanted to be a scientist?
Dr Satchin Panda: Yeah, so I was in India. I finished my undergrad in genetics and plant breeding. And that time, if you finish a degree in agriculture with genetics and plant breeding, then people expected you to become a plant breeder. I realised that, well, who would be a plant breeder in India? Because you have to work on rice or wheat, and both of them flower too early in the morning. So that means you have to get up, disrupt your sleep and go to the lab. So I actually I was running away from that life. I went, did a master's degree in molecular biology, what we call molecular biology here, it used to be called biotechnology. I worked in industry for a couple of years and that's when I realised that to rise up in ladder, either you have to be in management or in science in that particular company I was working for. So then I thought I'll choose science because you can always go back from science to management, but from management to science is not an easy task. So that's how I decided to do a PhD and ended up here in San Diego where I went to do my PhD in at Scripps Research Institute. It's a premier private research institute, very strong in chemistry, structural biology, genetics. And I did my PhD on circadian rhythms in plants. And then I during my postdoctoral training, I moved to mouse and then subsequently nowadays human circadian rhythm research.
Dr Rupy: So you've moved up the food chain from from plants to mice and now. Yeah, looking at.
Dr Satchin Panda: I wouldn't say that's a food chain from mouse to human is not a food chain.
Dr Rupy: No, no judgment of here. So let let's talk about, I mean, you're you're asked this question multiple times. I'm sure you're asked about it on every single podcast that you do. But I I guess just to anchor the listener, I mean, we've talked about time-restricted feeding for for quite a while in a few episodes. We had Walter Longo on, who I'm sure you know very well. Um, talking about it, but why don't we talk about circadian rhythms, exactly what they are to anchor the listener, and then we can talk about why you applied the the learnings from circadian rhythm to type two diabetes in particular and the impact on on glucose metabolism.
Dr Satchin Panda: Yeah, so circadian, the word circadian literally means nearly 24 hours or 24 hours rhythms. So circadian rhythms are daily timetables that are present in every single cell in every organ and in even in our every part of our brain. And these timetables are the master planner for our entire genome because they tell each of our 20,000 or so genes to turn on and off at the right time in the right organ. And this time-based program for genes to be turned on and off actually help in many different aspects. One is they improve our immune system so that we can better fight diseases and reduce sustained inflammation. They improve nutrition metabolism so that we can break down the toxins, repair DNA damage and also absorb and balance our internal nutrient state. They also turn on the repair and reset rejuvenation system. So that means we can repair our injuries because almost every day at a microscopic level, we go through a lot of injuries and damage to our body. So those are repaired. And then they also improve the neurotransmitter balance in our brain so that our mood and intellectual performance is optimized. So the circadian rhythms, although we immediately connect it to sleep and wakefulness, it's much more than that. It's in every cell and it optimizes when we have the right circadian rhythms, then it optimizes our physiology, metabolism, behavior, and even our gut microbiome.
Dr Rupy: And just talk us through, this is a relatively new science, right? We weren't thinking about circadian rhythms as it applies to human health for, you know, it's only it's been relatively recent. Could you describe in brief like how the science evolved over the last few decades and what that critical point was, I think it was in 2001 where there was an experiment that actually demonstrated why circadian rhythms are found in individual cells around different parts of the body, like the pancreas, the stomach, the digestive system, etc. and how that came about.
Dr Satchin Panda: Yeah, so we have been living with our circadian rhythms for 200,000 years ever since humans have been living on the planet, but we just became aware of it in the last 40 or 50 years. So the rotation of our planet around its axis creates this light dark cycle. So to adapt to that light dark cycle is extremely important for life. For example, even plants that just fix sunlight and carbon dioxide into the basic food in our food chain, they do have a circadian rhythm so that they can anticipate the first ray of light in the morning so they can prepare their photosynthetic machinery to optimize food production from the first ray. They also can optimize, anticipate based on the circadian clock, they can anticipate when the sun is going to go down and they can shut down their kitchen, their photosynthetic machinery. And the estimate is by having a circadian clock, almost all photosynthetic organisms, starting from pond scum to big banyan tree, they could fix around 10% more carbon on this planet because of the anticipatory effect of having a clock. For animals, we have to anticipate and adapt to day night cycle. During the light phase, the small animals have to go and hide from the predators. And the predators also have to be awake at night to go and hunt. We have to adapt to temperature fluctuation. So we all, all life forms, nearly all life forms on this planet have evolved to have circadian rhythm. The earliest, but we always thought that these rhythms are driven by light and dark. But are they actually driven or are they independent of light and dark? That was the question. And initially that question was actually asked almost more than 200 years ago when a French winemaker took a plant to his cellar and then found that the leaves went up and down in every 24 hours. And he was amused that there are these rhythms that are independent of day and night. And subsequently many other scientists discovered this light dark independent rhythms that are sustained under what we call constant conditions. So the definition of circadian rhythm is actually an endogenous rhythm that can sustain in the absence of environmental cues. And then people even in 50s and 60s, there are human volunteers, they would go to caves in Europe and completely disconnected from the outside world, temperature fluctuation because the cave temperatures are pretty constant. And they recorded their own sleep wake cycle and they found that they were actually going regularly to go to sleep and waking up in every 24 hours, 15 minutes or so. So that established that we humans also have circadian rhythms that are independent of light dark cycle. And essentially up to say early 70s were discoveries of circadian rhythms, existence of circadian rhythms in many organisms. And then the question was, if these are really endogenous rhythm, are there genetic basis to that? So in 1971, there was a famous study in Drosophila where they mutagenized Drosophila fruit flies and then showed that this mutant fruit flies have no circadian rhythm in activity or rest, or some mutants actually were waking up a little bit earlier, which we call period mutant with a short period, or they're waking up a little late every day, they had a long period. And at that time in 1970s, still scientists were not ready to accept that there is something like circadian rhythm that are encoded by the genes. So it took almost 15 years to for the scientific community to begin to accept that circadian rhythm is in fact a thing. And then I got into circadian rhythm. I was fascinated because I realised that the last century, most of the most of the biomedical research was based on what gene A does to gene B or what cell type does what, but there was no component of timing. And we know that the we are not the same creature between the middle of the day and middle of night. So I was interested in what we call biology of time, how biological systems keep track of time. And if we think about it, most diseases are diseases of mistiming. For example, cancer is a disease of mistiming because the cells instead of dividing, say in 18 hours or 24 hours, they begin to divide at 12 hours or 10 hours. So the the division, cell division becomes accelerated in a very simplistic way. Diabetes is a disease of timing because after a meal, our blood sugar is bound to go up and come down. And when it doesn't come down as quickly as in a healthy human and takes longer time to come down, then we diagnosed it as one aspect of diabetes. So I was interested in the biology of time and then I figured out that this 24 hours rhythms are very universal. They go from pond scum, single cell photosynthetic bacteria to all the way to humans. So the beauty is if you understand the principle in one organism, you may be able to apply that principle to humans, which is which is really exciting because cancer is a good example. The principles of cell divisions that people understood starting from bacteria can still be applied to cancer. So similarly, if we can understand the principles of 24 hours rhythm from simple organisms, we can apply that to human health.
Dr Rupy: Yeah, yeah. I've I haven't come across that way of thinking actually of diseases being a product of mistiming. It's a really interesting way of thinking about things. And and actually it makes a lot of sense when you put it in terms of, I mean, using diabetes, which is going to be the main stay of our conversation today. The velocity at which you see glucose entering the bloodstream, as well as the amount of time that you have an excursion of glucose outside the normal parameters of what you'd want in your bloodstream. These are all things that would drive someone to have a diagnosis of diabetes and all the, you know, ramifications of of having those issues too. Um, I I guess this is going to be an obvious question for for you to answer for for anyone in the know about the propensity of or the just the universality of how many people are suffering with either a diagnosis of type two diabetes or pre-diabetes. But what is the state of affairs when it comes to diabetes currently in the US and the UK? And why do you feel that time-restricted feeding or knowledge of someone's circadian rhythm is so important as it applies to this particular condition?
Dr Satchin Panda: Yeah, so in the last 25 or 30 years, I would say in the last 40 years, what we have seen is our circadian rhythms, if we simply define it as sleep wake cycle, because everything else kind of revolves around that, has seen a lot of disruption. When we say circadian rhythm disruption, then it's a very generic term and we let's define it more quantitatively. So we know that the modern world is possible because of shift workers, people who work in the night shift because they are the ones who take care of the society when the society is sleeping. And doctors, nurses, pilots, um, even service workers, truck drivers, all of them are shift workers. And we know that shift workers bear a disproportionately heavier burden of disease. So it was always the question whether these shift workers, they may not have access to healthy nutrition or they may be consuming excess alcohol or tobacco products to keep awake, keep themselves awake. That's why it's happening. So let's go back to the definition of shift work. So if you look at the international labor organizations definition of shift work, it's anyone who stays awake for two hours or more between 10:00 p.m. and 5:00 a.m. So during those seven hours, if you stay awake for two hours for one day a week, so that is 50 days in a year, then he or she is living the lifestyle of a shift worker. So why is that? Because if someone is staying awake for two hours and working, this person is likely staying under light. And that light will disrupt circadian rhythm. So the next day, the clock is delayed by one to one and a half hour. And if the person wants to come back to regular life, then it will take two more days to reset the clock back to its original state. So as a result, by just working, staying awake for two hours, two extra hours beyond your habitual sleep time, once a week, we disrupt our circadian rhythm for half of the week, the night is disrupted and then at least for two nights following that. And then the question is, what happens because of this? One thing is, for example, our going back to blood glucose regulation, our pancreas has a clock. So that means the pancreas anticipates that you would be eating breakfast at say 8:00 a.m. And accordingly, it prepares the insulin secretion process to be optimized so that in response to your breakfast, there is a good bolus of insulin that's secreted. If you eat your breakfast too early, then the pancreas is not ready. You may get a suboptimal insulin response. And if you miss the time, then again, there can be a suboptimal insulin response, but that's not very well demonstrated, particularly for breakfast. But at nighttime, similarly, your insulin producing cells are expecting when you go to sleep. And two hours before our sleep, melatonin levels begin to rise and melatonin levels again are indirect indication when the person is going to sleep. Melatonin inhibits glucose induced insulin secretion. So as a result, your insulin secretion system is slowly shutting down two to three hours before going to bed. And if you delay your breakfast and eat very close to bedtime, then you also miss the circadian optimized insulin secretion window. As a result, a late night meal leads to a prolonged hyperglycemia compared to the same bolus of glucose or calories earlier in the day. And this has been demonstrated for over 30 years now. So this is an example of how mistiming can lead to a very different glucose response. So now coming back to another aspect, we eat when we are awake. And when we when we are getting less sleep and particularly when you are delaying sleep, then we have more opportunity to eat. Then there is another aspect of our human nature that is our human civilization, the cradle of human civilization actually lies in the evening activity. What we do between 6:00 p.m. and midnight. Because during the day, we spend our time earning a living. And after evening, we are kind of free. That's the time when we feel intellectually, emotionally, and physically free. So we want to spend that time with our loved ones, with our family and friends. And one aspect of developing that bond is through food. So all of our in the ancestral time, the fireside chat after evening meal is where art, poetry, philosophy, science, politics, all evolved. And we continue to do that. In fact, the social media has actually given us more opportunity to extend that fireside chat to glowing pieces of rectangular objects and we chat through that. And with that, we also consume more food. So in that way, we do two different things. One is we are eating at the wrong time, very close to bedtime, which was not happening before. And second is we are also extending the number of meals or increasing the number of meals that we eat throughout the day. The third thing that happens is when we are sleep deprived, because we can go very late into the night, that gives us the free time. But in the morning, we have to do our regular job. That's when we lose our freedom. Our life becomes tethered to what time we have to report to work. So when you have reduced sleep, although you can reduce that morning fog by a cup of coffee, it does not improve your executive decision making process. So as a result, we make a lot of bad decisions throughout the day. And out of all the decisions that we make, irrespective of who is doing what kind of work, we all make a common decision, that is about food. What to eat, how much to eat, what combination to eat, and when to stop eating. And if we make bad decisions on any one, two or three aspects of this, then we'll end up eating bad food, excessive food, and wrong food at the wrong time. In a day, we take nearly 200 plus decisions about food and beverages. So you are more likely to make food related decisions, bad decisions if you are sleep deprived. So there are now three different ways that circadian disruption can directly or indirectly lead to compromising quality, quantity, and timing of your diet. And all these three will eventually lead to your health. So bad decisions about quality, quantity, and timing will eventually lead to dysmetabolism, obesity, diabetes, and metabolic disease.
Dr Rupy: Yeah, yeah. And this is something that you came to realise, I guess, initially through studies on mice where you would perform research where you would you would time restrict these mice. So they they could eat, I'll let you explain in a second because I don't want to bastardize it, but they would they would eat at libitum throughout a cycle that was above 12 hours or just any time of the day within 24 hours. And then you looked at ones that were time restricted and you found an improvement in the biometrics. Talk us through those experiments and and how you led to that hypothesis and how that's been replicated in in human trials.
Dr Satchin Panda: Yeah, so most of the human to understand human metabolic disease or to develop therapies, we do experiments in lab animals, particularly in mice and rats. And there is a famous experiment that is done in many labs around the world, we call it diet induced obesity, how changing the quality of the diet can trigger obesity. The idea is to mimic a western diet that is somewhere between 40 to 45% of calories from fat, 15 to 20% calories from processed glucose, simple sugar. And then a healthy level of protein actually. And then if you give this diet to mice at libitum, that is the mice have access to this food 24/7, then within 9 to 12 weeks, these mice become obese, they have excessive body fat, they even have fat deposit in their liver, and they show sign of glucose intolerance or early sign of diabetes. And this experiment has been replicated at least 11,000 times over the last 25, 30 years. So this is the staple experiment that all metabolism lab, almost all metabolism lab do. But almost 15 years ago, another lab, Joe Bass's lab at Northwestern University, found that when mice are fed this high fat diet at libitum or diet induced obese mouse models, they actually eat slightly more food during daytime. Mice are nocturnal, they are not supposed to eat too much food during daytime, that's their sleep time. They increase their eating by 15 to 20% during daytime. He made that observation, but then we asked, how much of this diet induced obesity is due to really high fat diet versus mistiming of diet? So we did a very simple experiment. We took identical set of mice born to the same parents in the same room, had the same genome, same microbiome. They ate the same number of calories, they ate the same diet. The only difference was the first group of mice ate at libitum or whenever they could. Yeah, so the second group of mice that ate the same number of calories from the same food were completely healthy. They weighed 28% less, their body fat was 70% less, and their cholesterol levels were almost in normal range, and their blood triglyceride levels were almost in normal range. And surprisingly, they actually could stay on an endurance test twice longer than the healthy mice that eat standard diet, healthy diet. So that was a big surprise. And they could stay on a rotating drum for a very long time. So their motor coordination was much better. And subsequently, we also found that these mice have much better sleep and they have much better gut or digestive system physiology. So the results were so surprising that we had to repeat it three, four times before we could publish. We thought this will be so dramatic that people will question us. And that's exactly what happened. For the first few years, I would go to a conference and scientific conference and people would come up to me and say, you know, your study doesn't explain the third law of thermodynamics. You must have done something wrong. You should go back and check this and that. And it was really scary because, you know, we knew that there is there is a benefit, but we didn't know how the benefit is coming. So we had to do a lot more work. But now this same mouse study has been replicated numerous times, at least 50 or 100 times by independent labs, they found the same conclusion. I must also say that eight hours is not a magic number. The reason why we did the eight hour experiment in the first one was my grad student, Christopher, who led this study, his girlfriend wanted him more than I did. So he she won. So he was allowed to be in the lab for nine hours. So that means the mouse could eat within eight hours. And people think that that eight hours is a magic number. So if you say time-restricted feeding or intermittent fasting, everybody says you should do eight hours eating, 16 hours fasting. You should go and ask Chris.
Dr Rupy: That's brilliant. So it's completely arbitrary based on his convenience.
Dr Satchin Panda: Well, so subsequently, we did the empirical experiment where we did 8, 9, 10, 11, 12 up to 15 hours. So the bottom line is somewhere between 8 to 10 hours is gave very similar results in mice. And 10 to 12 hours, the mice were protected from obesity and many other things, but they did not gain the endurance benefit that we see in 8 to 10 hours. So those are some of the differences. But essentially 8, 9 or 10 in mice are very similar. So sometimes we do 9 hours, we see very almost identical benefits. And we don't go below eight because that's when mice reduce their calorie intake and it will be difficult to figure out what health benefits are due to reduction in calorie, which we know will lead to benefits and also time restriction.
Dr Rupy: Yeah, I just want to I just want to summarize that because you've said a lot of things there that are fairly dramatic and I just want to punctuate that for the listener because they're they're pretty astonishing results there. So you fed these mice the exact same obesogenic diet that has been replicated in over 11,000 studies to to use your your words there in mice. And you found that just changing the timing by which you fed them the same diet that was all calorie and macronutrient controlled, you were able to avoid largely the obesogenic effects and even preserve some of their exercise effects, which I found particularly interesting because exercise as listeners to this podcast will know is one of the main drivers towards a healthy long lifespan as well as health span. So that that's amazing in itself. Um, and also you one of the the mainstays for for those who don't know too much about science and and uh maintaining an aura of authority is you got those results replicated independently in different labs so that you reduce the any element of bias there. So that that really does put a stake in the ground as to there's something going on here and now it's time to replicate now it's time to figure out what the mechanism is and see if this actually applies to humans as well because to to use a quote in your book, mice are nice, but humans humans are better.
Dr Satchin Panda: Yeah. We always ask whether mice are little humans or humans are bigger mice.
Dr Rupy: Yeah, yeah, exactly. So within the the spectrum of different time-restricted feeding windows, you've tried you you've tried everything between 8 and and 12. Where would you say is there a sweet spot? Is is there a sweet spot or is it is it is it pretty much the same?
Dr Satchin Panda: Well, when it comes to humans, we have to figure out what is feasible and what is healthy and you got to find that sweet spot. So for example, we know that reducing calories and avoiding all the alcohol is good for you, but then the sweet spot is maybe one to two drinks in a week or something like that. So similarly, we got to figure out what is the sweet spot. So in humans, the first thing is, do humans eat like mice? And initially people would say, no, we don't eat like mice. We eat three meals a day and so your results, even if it was true in mice, have no relevance in humans. So, and this is actually the criticism that we initially got and we said, okay, let's go back and see when people eat and how many times they eat. So we made a very simple app called My Circadian Clock. And the first iteration, the only thing people had to do was to open the app one click, take a picture of the food, two click, and then press save, three click. So that's all. They didn't have to say what they ate, how much portion size or anything, nothing. We just wanted an objective time stamped evidence that they ate or drank something. And it was up to us to determine whether it was water or whether it was black coffee, we would ignore those ones and then take anything that looked like they had at least five kilo calories or more as food. And we did that on 156 adults who are not college students and they were not shift workers. And what we found was nearly 50% of them had a eating window of 14 hours, 45 minutes or roughly say 15 hours or longer. And what is eating window is the window of time in which 95% of all the eating events within two weeks are likely to happen. So for example, suppose that one can say that yes, I eat everything within 10 hours. But if I say I eat between 6:00 a.m. and 4:00 p.m. today, and then Tuesday, I ate from 8:00 a.m. to 6:00 p.m. Wednesday, I ate from 10:00 a.m. to 8:00 p.m. and then I switch back, then our body is actually getting reset every day because the body is expecting food at the same time, but it's actually not getting food at the same time. So just like your jet lag, your body is going through what we call metabolic jet lag. So the best way is to figure out what is the roughly, what is the interval in which I'm most likely to eat. So that's why we come we come up with this definition. And in this example, although the person I'm eating within a 10 hour window every day, since the window is moving, our my circadian system is getting confused. So my actual eating window that the body is expecting food is somewhere between 6:00 a.m. and say 8:00 p.m. on any given day. So with that definition, what we found is 50% of adults eat for 15 hours or longer. And only 10% of adults eat consistently within a window that's 12 hours or short. So that means nearly 90% of people have the potential, have the head space to pay attention to when they eat and can try to eat within say 10 hours window because somebody who is habitually eating over a long period of time, we cannot expect him or her to quickly go down to eight or nine hours.
Dr Rupy: Yeah, I just want to punctuate that again as well, actually. So 90% of people, because the the circadian app that you've got that I think is available on Apple and and Google Play, it's like a big sort of public science research opportunity for for and you've you've had thousands of downloads. It's it's a really cool, simple app. And so that was designed really to figure out when people are eating and actually if if they say they're eating in a 10-hour window, is it actually 12 hours or 13 hours or whatever. And what you found from that was actually people, most people, 90% of people are eating out outside of a 12-hour window. Is that right?
Dr Satchin Panda: 12 hours. It means in any given week or two, your body is expecting food within that more than 12 hours window.
Dr Rupy: Right. And what you said also about the switching, just if you are able to maintain a 10-hour eating window, but that changes by a couple of hours every single day, 6:00 a.m., 8:00 a.m., etc. The circadian signatures that are embedded on your pancreas, your your digestive tract, etc, etc, that's enough to still cause disruptions. So you're not truly eating in a 10-hour window, it's more like a 12 or a 14-hour window.
Dr Satchin Panda: Yeah, it's almost like someone flying from London to Istanbul once a week or twice a week. You have like two time zone, roughly two time zone differences and that's what your body is experiencing. So.
Dr Rupy: Right. So the opportunity to experience some of the benefits of intermittent fasting is it's really not being realized by the majority of people, even if people are trying to maintain some fasting or some time-restricted eating windows themselves. And we'll we'll get into some of the benefits of what what those might be as well. But that that's the essentially the state of play at the moment.
Dr Satchin Panda: Yeah, so I guess the idea is to maintain a consistent window that doesn't change. So I mean, life is unpredictable, but still, if we can try to maintain a 10 hours window with say half an hour each on each side, some buffer, then that's pretty good enough. And if you can reduce it to eight hours and still maintain an hour window on each side, that's still awesome.
Dr Rupy: Yeah, absolutely. And you you mentioned some of the the reasons as to why it can lead to disruption to glucose homeostasis with disruption to sleep and everything, but I just wanted to to expand on the impact on the gut because something that I think is unknown to a lot of people is that your gut, your digestive system takes anywhere around five to six hours to process food through it. So if you are not eating within that window, you're never really giving your gut a rest. Is that am I right in saying that?
Dr Satchin Panda: Yeah. You put it rightly. So after your last bite of the night, your gut takes, your stomach takes around five hours to digest that food and then pass it on to the intestine, the next phase. So that means if if I finish my last meal at 6:00 p.m., then even if I'm not eating anything at all after that, my gut is still, my stomach would still be digesting that food till 11:00 p.m. at night. And then if you think about it, our gut is going through a lot of assault during the day because it's there is a huge amount of acid production that that's digesting everything that you eat starting from vegetables to the sashimi, that's uncooked meat. So your gut is also uncooked meat. And digesting that uncooked meat that you ate. So during this process, the gut lining also gets damaged. In a typical day, nearly 7 to 10% of the cells lining the gut are damaged, they need to be repaired or replaced. And that repair and replacement requires that your gut is relatively empty and it's not, your gut lining are not doing their job of absorbing nutrition so that they can repair themselves. And second is this gut lining repair requires growth hormone that's produced from the brain. And the growth hormone production happens only at nighttime or in your slow wave sleep mostly. So you got to align these two, slow wave sleep, growth hormone production, and your stomach has to be relatively empty for the stomach lining to repair itself. So that's why maintaining a long nightly fast and the fast should ideally start pretty early, 6:00 or 7:00 p.m. in the evening should be your last meal. So that gives the system enough time to empty the stomach and you should be in your bed to have the growth hormone released so that all of this can align and repair your gut lining. If the gut lining is not repaired, as you can imagine, over several days, the damage can accumulate. As a result, you can get what you call leaky gut. And it's not essentially your gut is leaking out all the food into your bloodstream, but small pieces of bacteria and allergy causing chemicals and other stuff can get into the system and can cause mild inflammation. And if it continues, that sustained inflammation can also lead to other diseases.
Dr Rupy: Absolutely. Yeah, yeah. So essentially, giving your gut a rest so it can prevent that hyper permeability that is a normal reaction to eating on a daily basis and that repair mechanism as well is super important. And I guess putting it practically, you know, if someone's eating in a 14-hour window, let's say, they have their last meal at 10:00, 10:00 p.m. It will take six hours for the the gut to digest and then they the gut suddenly has a rest at 4:00 a.m. and you wake up nice and early and you have a coffee with with milk and cream or a donut or whatever you're eating, granola, then your gut is back into action again. And so it's never really getting that chance to A, repair itself and and B, stop digesting food essentially. So, yeah.
Dr Satchin Panda: Yeah. So that's what is happening with late night eating, at least one aspect of it. And as I mentioned, also late night eating very close to your bedtime, your insulin system is not working properly. So your hyperglycemia may continue for a long period of time.
Dr Rupy: Yeah, yeah. Within that, if we were to to dive into someone who, let's say, is maintaining an eating window of around 10 hours, throughout the day, is it also beneficial to have defined periods of time when you do stick to a breakfast, lunch and dinner and you don't graze or snack in between those assigned meal times? Is there are there any benefits to that?
Dr Satchin Panda: Well, in practice, what we see is when someone goes through 14 to 16 hours of fast overnight, then they typically increase their first meal, you know, breaking of the fast. So that meal goes up in size. And breakfast is really an important meal in many different ways. One is breakfast is the meal on which many of us have good control because if we if you're eating breakfast at home, then you are in control of what you are putting in your mouth. Once you get out of the home, then you are at the mercy of which restaurant or which meeting you are attending that will feed you. So once you have a big breakfast, then your craving for snacks actually goes down. That's what we see in many of our clinical studies. So typically these people, they reduce snacking between meals. So they go from breakfast to maybe a modest small size lunch. And then they also have much better energy in the afternoon so they can avoid snacking. So typically what we see is they kind of adopt two or two and a half meal, breakfast and dinner, or breakfast and dinner with a small lunch. The snacking typically goes down. We haven't done any systematic study between people who are snacking six small meals within that 10 hours versus three meals. But there are other people who have done those studies. One study that came out of Israel among type one and type two diabetics showing that actually three meals within 10 hours, roughly 10 hours was much better in glycemic control than six meals spread over say 12 to 13 hours. So of course, there are two things going on, six meals spread over 13, 14 hours versus three meals within 10 hours roughly. But the bottom line is that study kind of says that three meals within 10 hours, even for type one and type two diabetics was much better because these patients could reduce their diabetes medication or insulin usage. And I thought that was really fascinating because almost every diabetes doctor will tell that try to eat small meals from the time you wake up till the time you go to bed. And this one took a very different approach. Stick to three meals, healthy meals within 10 hours window and still have 14 hours fasting and these patients were reducing their insulin usage and diabetes medication. Of course, the study has to be replicated, but what we see is in even in our studies, people with diabetes or early stage diabetes, early stage type two diabetes or pre-diabetes, they benefit from 10 hours time-restricted eating.
Dr Rupy: Yeah, yeah. If if those are found to be true and replicable, um, that will really revolutionize how the advice that we give as doctors to patients, um, because the aim of the game just for the listeners is to try and reduce the amount of medications that we give patients, particularly insulin, because too much insulin can have anabolic effects and and other undesirable side effects as well. So if you can reduce the amount of insulin being given via a pump and the different types of insulin, then that's actually a win for everyone. So we've talked about the benefits of this particular way of eating through the lens of the microbiota, sorry, the the gut, the digestive system, probably with spillover effects on the microbiota as well, the impact on on insulin release. What are some of the other mechanisms by which intermittent fasting can can potentially benefit people through, you know, fat deposition or muscle breakdown? What what are the other things that that interest you the most?
Dr Satchin Panda: Well, if you look at the number one and two causes of death or disability, it's cardiovascular disease and cancer. And that's why we are very interested in how to reduce the risk for cardiovascular, cardio metabolic disease and also reduce the risk of cancer, accelerate the prognosis of cancer and also rehab. So prehab, prognosis and rehab for cardio metabolic disease and cancer, those two areas will have the biggest impact on human health. So when it comes to cardio metabolic disease, the I guess the first few stages where things can be reversed are obesity and pre-diabetes. And for obesity and pre-diabetes, time-restricted feeding or intermittent fasting can directly and indirectly benefit in many ways. One is in humans, unlike in mice, in humans, when humans reduce their eating window to say eight to nine or 10 hours, mostly eight hours or less, then they inadvertently reduce their caloric intake by as much as 20%. And this is very dramatic because reducing calories by 20% by counting calories is very difficult. Even long-term studies funded by the National Institute of Health in the US, which targeted to reduce calories by 25% in healthy humans over two years, they found that they could reduce only by 12% by counting calories. So now the question is, by counting, instead of counting calories, if you count time, and all of us can count time, we don't have to read levels. If we can inadvertently reduce calories by even 15 to 20%, that's a pretty good calorie reduction for diabetes for obesity management. Then second is for pre-diabetes, which affects now one in three adults in the US and roughly one in three adults in UK, I would suspect. Then studies, human studies have shown even without weight loss, if people eat within a short time window, eight hours or nine hours, something like that, then they can improve their beta cell function and reverse pre-diabetes because you can, I mean, people can reverse their pre-diabetes, but once you are settled with type two diabetes, the truth is it's very hard to reverse and be medication free for your life. So the reversal of pre-diabetes is possible by time-restricted feeding. Obesity management is possible by time-restricted feeding. Then when it comes to type two, early onset type two diabetes, then there are now ongoing studies and then the study that I mentioned from Israel showing that, yes, they will benefit type two diabetes patients with or without even insulin. Then what when it comes to cardio metabolic disease, the other two things are blood pressure and triglyceride. And one surprising thing that we find in most time-restricted feeding studies so far in humans is time-restricted feeding or intermittent fasting disproportionately benefits blood pressure reduction, particularly diastolic blood pressure, which is very difficult to manage with medication. Systolic blood pressure, of course, reduces, but then the diastolic is the one that also sees a lot of benefits from time-restricted feeding. Then the next is triglyceride and lipids. We think that it might take longer time with time-restricted eating and time-restricted eating alone may not be sufficient. We may have to combine that with some improvement in diet quality to achieve that lipid profile. But some of the results that we are seeing, early results from NMR lipoprotein profile is we're seeing improvement in VLDL cholesterol and maybe some apoB. Of course, the jury is still out because small studies, we have to see multiple studies. So in this way, I'm very hopeful that the overall cardio metabolic disease risk can be reduced to some extent. Let's be frank, I mean, when a person goes from healthy to diabetes, then the health, the total healthcare cost for that person in the US goes up by $9,000 per year. And if the person has metabolic syndrome, which is three out of five different complications, then the healthcare cost is even more. And in the next 10 years, most of the nearly 60% of the pre-diabetic will transition to type two diabetes. So now if we do the math, even if intermittent fasting, time-restricted eating can prevent 10% of the pre-diabetic to transition to pre-diabetes, that itself is several billion dollars in healthcare spending savings and also several years of healthy life for those individuals. Now, we can extrapolate it to cardio metabolic disease and do the math. The bottom line is, yes, we can move the needle. I'm not promising that it will benefit everybody. It's almost like going to a restaurant menu. If you even if there is there are 10 items, all of them are pretty good. We have certain preferences for certain items. So some people will find it easy to adopt, some people may not find it easy. But the bottom line is it is on the menu to reduce your risk for cardio metabolic disease. For cancer, there are many studies now showing there are benefits. Of course, now cancer is also linked to obesity and metabolic disease because hyperglycemia alone or hyperglycemia with obesity also increases risk for many cancers. And also cancer survivors who have hyperglycemia and metabolic diseases, they're also at a high risk for relapse. And if we can manage these, then we can reduce cancer risk and also reduce relapse risk. So in that way, I think this circadian rhythm has given a new insight and also new opportunities for prevention, management of these diseases that will benefit millions of people worldwide.
Dr Rupy: Yeah, absolutely. I I I totally agree with that. I I guess you mentioned um one of the side effects of applying time-restricted eating or windows um in practicality to to humans, they they tend to eat less. Are there studies that are able to separate out the effects of the calorie restriction from true uh uh time-restricted feeding without the inadvertent effect of of calorie restriction? Like have there been any studies looking at people within a metabolic chamber where you can actually see everything in terms of their calorie consumption and just change the windows in the same way we would do with mouse studies?
Dr Satchin Panda: Yeah, so there are few studies and then the most exemplary study is from Courtney Peterson published in cell metabolism where he fed people with pre-diabetes a diet that maintained their body weight. The aim was to maintain the same body weight, but feed them within 12 hours or six hours. And what she found was when these people ate within six hours, they improved their glucose sensitivity and improved their blood pressure regulation. So that's a, of course, that's a short-term study because you cannot keep this control study for over months. But even with this short-term study, after controlling for body weight and caloric intake to maintain that body weight, she found these benefits. So that's the most promising in humans. Coming back to other studies where caloric restriction and time restriction were combined, there's one study that just came out from China which made a big headline and unfortunately headline, but actually what was interesting in that study was at baseline, these patients already had a 10 hours eating window. And their target was to reduce it to eight hours eating window. And when you go from 10 to eight hours, we know that even in animals and in humans, there's not much difference. I mean, there is some there may be some difference, but you need large number of people to see that difference. Whereas this study, I think was not powered enough to see a difference in the benefits of time-restricted eating when someone changes from 10 hours to eight hours. On top of that, all patients had to reduce their calories by 25%. And they did, they reduced their calories by 25%. And um, the conclusion was those who did caloric restriction and time restriction were as healthy as those who did caloric restriction alone. So then New York Times declared that time restriction doesn't add any benefit. This is the challenge with with big media because even for many scientists, it becomes very difficult to go through the nuances of this scientific papers, clinical trials and how the power calculation was done and what is the baseline characteristics of these patients and to dissect that to come up with a clear opinion. So I don't blame the reporters, but it's unfortunate things that happen. And we have seen this in many studies. There will be studies coming out saying, low dose aspirin has no benefit. But actually, we know, cardiologists know that those who already have one MI event, low dose aspirin is extremely beneficial. So it's all depends on context. What's your baseline and where you are going. So I think the there is very clear data from hundreds of studies now that time-restricted eating can benefit, whether the benefit is coming through caloric restriction or through directly, that's a that will depend on the condition. So for example, no one has looked at acid reflux and time-restricted eating, which can, which we know anecdotally from all of our patients that they do see benefits and hopefully those studies will come up. And how whether time-restricted eating can be combined with chemotherapy to reduce the adverse side effect of chemo so that people can tolerate and complete their chemo during cancer treatment. So those things also have to be looked into. So there are many areas where this can be tested. The simple weight loss may not be enough.
Dr Rupy: Yeah, at the same time, last week, there was another study that came out in mice showing um different groups of mice that went through the same caloric restriction. They had the exact same reduction in calories by 30%. Um, and then they were compared against an ad libitum fed group. So the experiment is very simple. You reduce calorie and then spread the calories in eight equal meals spread throughout day and night so that you can see the clear benefit of caloric restriction. Because in most caloric restriction studies in mice, the reduced calories is given in one bolus at any given, usually in the late afternoon, and mice eat that calories within two hours. So they're going through two hours of time-restricted eating. So this experiment asked, okay, so if we spread the calories, then what happens? If we give the calories within two hours, what happens? If we give the calories within 12 hours by six equal size meals, what happens? What they found is all of these CR mice ate the same number of calories. But the difference was the CR mice that spread the calories over 24 hours, they lived 10% longer than the ad libitum fed mice. Good news. But the CR mice that reduced the time window to 12 hours, whether it's day or night, they lived 10 more extra percent. So they lived 20% longer. And then the CR mice that ate the same number of calories but ate in their habitual time of nighttime when mice are supposed to eat, they lived 35% longer. So this is a clear example where CR alone extends lifespan by 10%. But if you combine CR and TR and feed mice at the right time when they're supposed to eat, then you can extend lifespan as much as 35%. That's the median lifespan extension.
Dr Rupy: Yeah.
Dr Satchin Panda: I think and what is interesting is in all these CR groups, the body weight was identical. So the body weight was not predicting how long the mice could live. By the same token, you know, this just this is a first study, so there's not enough molecular data to digest and say, hey, we can look at this blood biomarker and that would predict whether this reduced weight will lead to long lifespan or not.
Dr Rupy: That that sounds fascinating. I think we'll have to wait until we can actually replicate that if at all in in practically in in human subjects. But it seems that like you said earlier, we have a selection of different tools. We have calorie restriction, we've got time-restricted feeding, we have exercise, we have all these different options. And I think it's about trying to fit that in conveniently into one's lifestyle such that they can reap the benefits of those, which we know of. And I think the the details on exactly, okay, how much is it related to the time-restricted feeding window versus calorie deficit is sort of up for discussion. And I think there's always going to be a bit of a healthy debate on that. Putting it practically, because I get asked about this a lot, um, as a former shift worker, I've now taken the decision not to do any more night shifts for the rest of my life if I can avoid it. Uh, but certainly someone who travels quite a bit. I I guess you're asked this quite a bit as well. As a night shift worker, considering all we know about the detrimental effects on one's physiology from staying up at late at night and then switching uh circadian time, the circadian rhythms or disrupting it, how can we avoid or at least mitigate against those issues with the different tools that we have, when we eat, light exposure and and exercise, I guess.
Dr Satchin Panda: Yeah. So I guess we can um let's just begin with regular folks, not night shift physicians.
Dr Rupy: The regular folks, yeah. Well, from your definition that I was quite surprised about, there's probably more, there's.
Dr Satchin Panda: Everybody is a shift worker.
Dr Rupy: Exactly. Yeah. I'm thinking about non-card carrying.
Dr Rupy: Okay, yeah.
Dr Satchin Panda: Well, so I guess there are six different, six basic steps, I would say. Uh, number one is your day actually starts the night before when you go to bed. So try to go to bed at a consistent time and be in bed for eight hours so that you can get at least seven hours of sleep. That means on your calendar, daily calendar, set aside eight hours in bed. And because sleep has numerous benefits including synaptic plasticity, learning, memory, brain rejuvenation, detoxification, a lot of benefits. Then after waking up, wait for at least an hour or two before the first bite of the day because this is the hour when your digestive, although you just woke up, your digestive system, your endocrine system, your hormonal systems have not adapted to waking up and being in the day state because the night hormones, for example, melatonin is still declining, not come to baseline. And the day hormones, for example, cortisol has begun to spike and the hormonal states and the digestive system is not ready for digestion. So avoiding food for one or two hours is the step two. And then the third one is to have your breakfast or the meal after overnight fast at a consistent time. And then starting from breakfast, eat all your calories within 8, 9, 10 or max 12 hours, not longer than 12 hours. Because this time-restricted feeding or intermittent fasting has been shown to have many benefits. It aligns your digestive system and nutrition usage with circadian rhythms in neuroendocrine rhythms. It also improves fat oxidation during the fasting time followed by all the anabolic processes. So that's number three. And number four is try to be outdoor for at least 30 minutes during the day under daylight. You don't have to be standing under sunlight because even in London in a cloudy day, you get 5 to 10,000 lux of light. And what you need is at least 1,000 lux of light for 30 minutes to an hour because light, particularly daylight, entrenches our brain circadian clock, reduces depression and lifts our mood. So is the natural antidepressant that's plentiful, free outdoor. You just have to step outside. Um, then the next one is number five is exercise because exercise is truly medicine. We still don't understand how it does, but it has huge pleiotropic impact benefits in many organ systems. And particularly from circadian rhythm point of view, what we have seen is late afternoon, early evening exercise is much better than exercise in the morning or very late night because that's the time when your muscles are prepared to do exercise. Your flexibility and is much better so that you have less risk for injury. In fact, more world records are broken in the late afternoon, early evening than any time of the day. So you can break your own personal record by doing exercise in the afternoon. And then the last one, number six is to wind down because your evening decides rest of the day. So two to three hours before bedtime, avoid any food and also avoid any bright light because bright light can suppress melatonin, the sleep hormone melatonin, and it can delay or disrupt your sleep. So being in a relatively dim environment, which is maybe less than 40 lux of light, which is typical light level in an old English home, whereas the light level in a typical grocery store is 1,000 lux, that's pretty high. So that will help. So these are the six simple ideas and hopefully out of all of these six, if someone adopts time-restricted eating, then automatically you are adopting avoiding food for two to three hours before bedtime and you're also adopting one hour fasting in the morning. And time-restricted eating alone is also seen to improve sleep. So that's why this is one thing that you can do to improve four different aspects of this circadian rhythms.
Dr Rupy: Yeah, yeah, that makes a lot of sense. I mean, uh, if you can knock off a couple of those things by doing one thing or having one guideline as to when you eat, uh, it it definitely makes a lot of sense. So consistency, not eating too early in the morning, straight off the waking, 10 hours of time-restricted feeding and making sure you are exercising, winding down and exposing yourself to adequate light during the day. Now, the pushback I'm going to get is this is great if you have uh, you know, nothing, no obstacles in your day-to-day. So I I like, you know, I always say in talks that I I I give, I'm like, look, these are the characteristics of what we want to try and aim for, right? This is perfection over here. If you can achieve all of them, fantastic. The the solutions are simple. The implementation, that's the hard stuff. That's, you know, keeping the consistency for everything. I struggle with it. I mean, this week my waking up time were were all over the place. I I track my sleep every day. I can see the the differences in terms of when I wake up and the effect that has on my cognitive abilities the next day. So, I guess given your experience, what what do you have any advice for people who who have such disruption to their day-to-day?
Dr Satchin Panda: Yeah, I guess we accept that there will be disruption from day to day. So that's why starting from mouse experiment to humans, we are actually we also see how much of disruption is tolerable. So for example, in mouse experiments, we would give mice five days of time-restricted eating and then the weekends were off. So they could we used to call them the weekend parties for the mice and then they would eat more than even the ad libitum fed mice. They gorge food. But still they were benefiting, they were getting almost 80% benefits. In human studies, particularly one we are doing with shift workers, night, 24-hour shift workers, the firefighters, we are also finding similar results. If they could do five days of time-restricted eating, 10 hours during their preferred window, we don't have any restriction, they can choose any 10 hours window, then they're still seeing many cardio metabolic benefits. So those are some of the things to keep in mind that if you miss it, it doesn't mean that you fell off the wagon and you cannot get back on. It's tolerable. And again, at the end of the day, your lifestyle is what, when and how much we eat, sleep and exercise. And if you compromise on one aspect, you always have opportunity to make it up by doing a little bit more on the other. So for example, if you sleep less, then maybe there's a day to go, go for a brisk walk outside. Although you may be so sleep deprived that you may not go for your resistance training or running, but go for a good walk under daylight, then next day automatically you will compensate by sleeping, having a good night's sleep. So we have to keep that in mind that lifestyle is beyond time-restricted eating.
Dr Rupy: Yeah, yeah, exactly. I I sometimes I think, you know, we talk about this stuff on the podcast and it sounds quite puritanical. And I think people need to realize like there is a push pull of life. And part of that is the enjoyment, you know, the late night eating at the weekend or catching up with friends or like I'm getting married this year, so I'm going to be on my, uh, we call it stag over here. You guys call it bachelor party. I'm actually going to be in America. And uh, I I know that's going to be disruptive to my sleep and a whole bunch of other things as well about what I'm going to be eating and all, you know, the accessibility of greens that I'm habituated to eating every single day. So, you know, all these different things, I think you just have to take with a pinch of salt so to speak and just enjoy the ride. But have a sense of like what you're able to achieve consistently or as consistent as you can be with that. And within the shift work, sorry to double down the shift working element though, within the shift working practice, the shift workers, is there evidence for a practice of having a meal at the start of their shift and a meal at the end of their shift and not eating during the actual shift if possible? Or is it just whatever you can achieve in terms of a 10-hour window?
Dr Satchin Panda: Well, it's a very difficult question because shift work is very fuzzy. Right? So there are, although we did the study among firefighters in the US, the career firefighters in the US who do have a regular job, that's only 250,000 firefighters in the US out of a million firefighters. The other 700 actually are temporary, so they don't have a regular schedule. Among those career firefighters, again, 70% of them do 24-hour shift. And the rest do 12-hour shift or even 48-hour shift or 72-hour shift. The shift, even among 24-hour shift, the shift can start at 8:00 a.m. in some fire districts, can start at noon and can also start in the evening. So it becomes difficult which shift we have to look at. And as you have seen in medicine, in the US, I have seen in the same medical school, different departments will have very different schedule for their residents and fellows. So unless we standardize shift work, it becomes difficult. But the bottom line is what we are finding, all shift workers should have access to darkness. Because when you come home, irrespective of which shift you work, you have disrupted sleep and you need a completely dark room with noise cancellation or background noise to help you sleep because your sleep is very thin, you're more likely to wake up too many times during the day. And you have to have a supportive sleep environment. Coming back to food, again, it depends on what kind of shift you are on or what you are working on. So for example, we don't want people to be so weak. In firefighter study, for example, we didn't want them to be feeling low energy when they're getting their 10th call at nighttime. So we said, okay, so it's up to you, you can go and eat. But surprisingly, what we found was nighttime fasting boosted their energy levels so that they could do that 10th call without having to eat a snack before that 10th call in the morning. So, of course, it took a while for them to adjust to that, but they could do it. And the other thing is, you know, people always ask about coffee. Is coffee is going to break your fast and what is the rule? And for shift worker particularly, I mean, if you are sleepy, if you're a surgeon and you're going to put somebody under your knife, you better be awake. So when it comes to, so the the the rule about coffee or food is if it involves public safety or somebody else's life, you're okay to have your coffee whenever you want. Second is, if your job depends on it, and also if you're finishing the shift and driving back home, it's better to be caffeinated and awake than. Second is if your job depends on it, and then the third one is if this is the only love in your life, okay, you can have it.
Dr Rupy: Yeah, I'm glad you said that. I love my coffee. I have a black coffee in the morning, but I actually wait for a good like hour and a half before I enjoy it. Um, just because I don't want to have the same sort of cortisol spike and stuff as soon as I wake up. I just want to ride it out and just have water instead. So, yeah. I'd love to know about what your regime is in the morning actually. Like you must get asked a lot about your supplement regime or like what you tend to break your fast with or, you know, that kind of stuff.
Dr Satchin Panda: Well, to be frank, just like you said, you you had a very tough, you know, when you are training for physician or your early days as a physician, similarly in college and PhD and postdoc, I had no hours and I was at least, I guess, 10 kilos more than what I am right now. And then I think right after the mouse study, it was really eye opening that if mice could improve their health so much and if we really wanted to translate to humans, then why should not be we should be the big mice in the lab. So we started doing. So, you know, I try to eat within 10 hours and it's mostly two meals, a big breakfast and then dinner usually. And then in the daytime, if there is any opportunity for a small salad or fruit and sometimes that's not there. And it makes a huge difference because for a lot of time, I used to have sleep problem or acid reflux problem to a point that almost two to three times a week, I would take acid reflux medication and that's completely gone for almost 9, 10 years now. Sleep is much better. My joint inflammation has gone down. There was a point I could not, I could feel pain in at least one part of my body in every week and now that inflammation has gone down. And another thing is when you do time-restricted eating, it also improves your nutrition because as I said, breakfast is the best meal, you have good control. And if you're not eating and drinking late into the night, you also reduce your alcohol intake, dessert intake, simple sugar intake. So that also improves your nutrition quality. So that's kind of my routine. And then when I travel, I avoid food during flight. And even for a long transatlantic flight, if we avoid food, then you reset to the new time zone much faster and then there is very little jet lag. So these are some of my usual routine. And again, supplements and other stuff, those are very personal stuff because, you know, some people need more calcium, some people need some vitamin D, almost everybody needs vitamin D. And depending on what um deficiency you may genetically have or historically have, then that should come in. But again, you know, supplements are also another weird side of medicine where different, I think different people need different set of supplements. So that's why clinical trials or long-term cohort studies on supplements usually don't give you good signal to noise ratio. And those things have to be again personalized.
Dr Rupy: Yeah, yeah. I'm pretty bullish on the idea of food first, but I definitely appreciate that people need supplementation in today's day and age. Uh, certainly vitamin D3, um, omega-3 appears to have a number of benefits. I've seen that anecdotally, uh, clinically as well as in in studies as well. Um, but I I always wonder about people's personal sort of supplementation habits, uh, and and and how they translate the science themselves. And you're right, it is very personal.
Dr Satchin Panda: Another thing is, you know, um, another hidden um pandemic that's going on is uh the sterile food that we eat. Um, I mean, most of almost every food that comes pre-packaged doesn't have even a single microbe, I would say, literally on them. And if you contrast that to our ancestors or even few years ago when even the fruits and vegetables are heavily irradiated to make sure that there is no microbe growing on them. So our intake of microbes that come naturally with food has substantially decreased and COVID has even made it worse because now we are so scared about sanitation that our touch, our microbial ingestion or diversity might actually decrease. And even the food that we process food, even if you're eating a ketogenic bar or even a regular croissant or anything that you eat, that you buy, if you buy and leave it on your counter top for a week or two, nothing happens. So my my idea is if it is so bad for the bug, how good it can be for your gut. So that's another thing that we have to keep in mind that once in a while, just go and try to mindfully eat some food that has not been irradiated or thoroughly washed with Lysol or something else.
Dr Rupy: Yeah, yeah, exactly. Have you taken steps to eat more microbially uh more diversity in terms of your food? Like do you have like uh kefirs or micro rich?
Dr Satchin Panda: We just make our own yogurt at home and then I have we have a small garden, you grow um any vegetable that you eat from your garden has enough microbes.
Dr Rupy: Oh, nice. Okay. Yeah.
Dr Satchin Panda: So any tomato or even herbs or everybody, even if you are in an apartment, you can always grow some herbs and tomatoes in a pot.
Dr Rupy: Absolutely. Yeah. That's what we try and do here actually. The first thing I'm going to do uh when I get a garden eventually in the next year is uh start growing my own because I think it's super important. And just to get connected again with the uh the soil and and where food comes from, I think it's super important. Satchin, this has been brilliant. Thank you so much for spending time with us and and talking about your book. The book is is fantastic and I I wonder what the next title might be, where which uh which part of the body are you going to apply the circadian code to? That's brilliant.
Dr Satchin Panda: Well, we are very excited about diabetes because, you know, even in in the context of COVID, one of the things that that is becoming clear is post-COVID syndrome involves for many people, disregulation of glucose metabolism. And in the US with a population of 340 million people, if the projection is nearly 150 to 200 million people will be eventually infected with the virus and one in four will have post-COVID syndrome. That's millions of people with post-COVID syndrome who may have dysregulated metabolism in the form of hyperglycemia. So, I guess still this is a pretty good approach to manage hyperglycemia. And it'll be interesting to see test whether time-restricted eating can manage hyperglycemia in post-COVID syndrome. That's.
Dr Rupy: Yeah, absolutely. Yeah, that would be that would be fascinating to see actually. And especially with the rise of people using uh continuous glucose monitors, um, and the the number of private companies that are making it more available to people. I think uh better data and just an idea of how your body is personally responding to certain foods will hopefully accelerate people's knowledge around what other practices beyond changing the food itself can help with their body's um response to to glucose. So, yeah, super super interesting. Definitely one to watch.