Professor Felice Jacka: But just this knowledge that if you feed your gut, you're going to be doing good and you don't need to know the detail of which bacterial strain is doing what. You just need to know that your gut bugs need fibre to do what they do. If you don't have enough fibre, they can't do what they do.
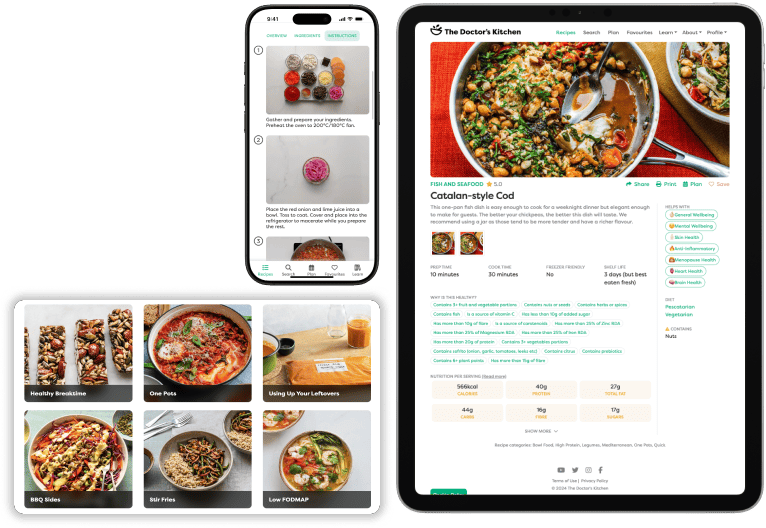
Dr Rupy: Welcome to the Doctor's Kitchen podcast with me Dr Rupy where we discuss the most important topics and concepts in the medicinal qualities of food and lifestyle. These are some of the things that I've written about in my latest book Eat to Beat Illness and today I'm speaking with Professor Felice Jacka about her new book Brain Changer and how diet can save your mental health. Prof Jacka first came on my radar when I heard of the SMILES trials and we're going to actually talk about this a little bit later in the pod. Her book tells the story of why we need to consider our food as the basis of our brain and mental health throughout our lives. There is a lot of evidence-based, safe dietary and lifestyle change that we as practitioners can be confidently discussing with our patients and that's what we hope to chat about today. You can find all of this information and more at thedoctorskitchen.com, subscribe to the newsletter for weekly science-based recipes and listen to the end of the pod for a summary of our discussion and how to improve your overall wellbeing. Professor Jacka is the director of the Food and Mood Centre at Deakin University in Australia. She is founder and president of the International Society for Nutritional Psychiatry Research and pioneering a highly innovative programme of research that examines how individuals’ diets and other lifestyle behaviours interact with the risk of mental health problems. We're doing something a little bit different now on the Doctor's Kitchen podcast where I actually cook my guest a recipe live. Now you can catch this recipe on YouTube and thedoctorskitchen.com if you want to check it out. Unfortunately, the audio didn't work that well this time, so if you're finding it difficult to listen, then you can just skip to about 25 minutes in where we switch mics and we do a standard podcast. We will be brushing up the audio for future episodes so you can hear everything a lot more clearer, but unfortunately this time it just didn't work out. So if you're struggling, skip to 25 minutes in and the audio is a lot more clearer. Otherwise, enjoy the podcast. Welcome to the Doctor's Kitchen with me Dr Rupy and today I have the absolute pleasure of cooking and speaking to, cooking for and speaking to Professor Felice Jacka. Welcome.
Professor Felice Jacka: Thank you.
Dr Rupy: How are you?
Professor Felice Jacka: Jet lagged, but okay. Hungry.
Dr Rupy: Now you're the author of a fantastic new book. I've read it cover to cover as you can tell because I mean there's, yeah.
Professor Felice Jacka: So you're not making it up. No, I'm not making it up.
Dr Rupy: Brain Changer. Tell us about it.
Professor Felice Jacka: Okay, so, well, starting with my PhD back in 2010, I I guess I pioneered this field of research that we call nutritional psychiatry and it focuses on the link between diet and nutrition and mental and brain health and it looks at how we might prevent these mental illnesses and brain disorders, but also treat them using nutritional approaches. And I was asked many years ago to write a book and I said, no, no, we have to wait until we've got the data from the trials to say if we change diet, we can change depression because once we've got that, we've got the whole picture and then we can give people advice. So when we published the SMILES trial in 2017, that sort of circle was finished if you like. I'd done the work in from pregnancy to early childhood, adolescence, adults, older age, and then the trial and I right, it's time for the book. And the other reason too is that people keep on asking for information and it needed to be something that was accessible that people could understand readily.
Dr Rupy: I remember you actually writing that anecdote in the section on the SMILES trial because I thought that was very admirable of you to not write a book even though the offer was there until you'd actually done the intervention trial.
Professor Felice Jacka: That's right. You need and that's I think the key, the fundamental is that I really care about rigorous science and there's so much misinformation out there. There's so many diet gurus, particularly in the US who are promulgating I think quite often misinformation and information that's not evidence-based or the evidence is very cherry-picked.
Dr Rupy: Before we start talking any more, I'm going to tell you what we're going to be cooking. It's going to be a modified version of one of the recipes in your book. It's the open Mediterranean sandwich. So we've got some beautiful sourdough that you already love the look of. And this is kind of the thing that you would eat for lunch, right? So quite light and yeah.
Professor Felice Jacka: Yeah, yeah. And our whole team, you know, we had the Food and Mood Centre and we sit and have lunch together almost every day at a big table and we all just inspect everybody else's food and go, oh, that looks amazing, can I have some of that?
Dr Rupy: It sounds like I definitely need to pay a visit. That's definitely the kind of place I would love to work in. Okay, yeah, so we're going to be making a modified version of that Mediterranean open sandwich. So we're going to do some red onion, some beautiful local mushrooms that we've got here, some shiitake, we've got some Lincolnshire, I think, some portobello mushrooms. So that's going to be like sort of the base of the meal, but we're also going to throw in some beautiful green beans and I'm also going to be toasting some hazelnuts as well. Good quality fats in, the ones that we talk about. We'll do that at the start and then I'll chop them up roughly afterwards. And we're going to be using, you use a dukka, which is that Egyptian sort of spice blend with coriander seeds. We don't actually have that over here very popular, but za'atar I think is a good sort of alternative. It's got sesame seeds and a whole bunch of other things. And I've already pre-cooked some some black-eyed peas here. You can get these in cans and sort of like tetra packs as well. Just drain them, rinse them, good to go. But I actually prefer cooking them from scratch because you've got a little bit more texture and stuff.
Professor Felice Jacka: Yeah, yeah, I agree.
Dr Rupy: So whilst I'm toasting these, tell me about how you got into this because you didn't go straight into research on nutrition.
Professor Felice Jacka: I had a very a misspent youth and came at this from a very circuitous pathway. So my first degree was in fine art. I was an artist and that was way back in the 80s and then because of my personal experience I guess of what we call common mental disorders, so that's depression and anxiety, I was very interested in psychology and I went back to university in my 30s to study psychology. And as I was studying, I I sort of increasingly realised that I wasn't that interested in being a counsellor, a clinician, but I was very interested in research and in statistics because I'm a big nerd. And so I started when I was doing my undergrad, I sort of did some interning and then some paid work as a research assistant in a new little research lab that had been set up. And from there I I, you know, finished my degree, did my honours in looking at depression and osteoporosis and, you know, using epidemiology. So epidemiology is when you collect lots of data from people and you use statistics to put it together. You don't do any experiments though. And while I'm doing this, I'm sort of learning about this whole field of psychiatric research. And I'd always been really passionate about food and always had this, you know, belief that food is sort of fundamental to health and certainly in the wider area of medicine, of course, we've known for a very long time that what you eat is really important to your risk for chronic diseases.
Dr Rupy: Was that sort of influenced by your background? Because I remember reading the book that your your parents were naturopaths, is that right?
Professor Felice Jacka: That's exactly right. So in that, in that sense, yes, because they had a real interest in in diet and nutrition. But in another way, there was a lot of what they said and did that was at odds with sort of evidence and good science. And as I trained, I realised just how divergent they could be.
Dr Rupy: It's like my parents and I grew up in an Indian household and Ayurveda features quite a bit. There are good parts and there are things that are at odds with what I believe as well.
Professor Felice Jacka: I think with naturopathy, it often can prompt, you know, hypothesis testing and it's a good starting point for research, but it certainly there's a lot that is over extrapolated, simple solutions to complex problems and we always know that that's incorrect. And I was just fascinated to realise that in psychiatry, there really wasn't this field, this body of research that had looked at the role of diet and nutrition in mental and brain health. And it was around that time that there was increasing focus on this field of research and science called psychoneuroimmunology. So this is really about how your immune system influences your mental health. And vice versa, how your mental health influences your immune system. And it was really putting paid to this idea that your mind and your body were separate. And we were really starting to get the point that, you know, we're one highly complex, fully integrated system. So the the old ways in which psychiatry was viewed as just everything happening in the brain and in the head was not being supported by the new evidence. But also at that time, there was a lot of neuroscience coming out of the US looking at how we might influence what we call brain plasticity using diet and exercise.
Dr Rupy: So this is fairly new as well, the the knowledge that our brain is fairly plastic or it maintains its plasticity rather than being static after.
Professor Felice Jacka: When I was growing up, the the wisdom was that you had a set of brain cells that you were born with and you only lost them over time. And then I think in about the late 1990s, neuroscientists recognised that there was at least two areas of the brain that puts on new brain cells all the time. And in doing so, that supports the function of that particular area of the brain. So the area that we're particularly interested in is something called the hippocampus, which is two little structures side by side in the middle of your brain.
Dr Rupy: Seahorse monster.
Professor Felice Jacka: Yeah, that's right. And they're really, really important for learning and memory. And this is not just in old age, but, you know, right from the start of life. But we also know that that area of the brain is involved in mental health as well. And the neuroscience studies in animals were showing that if you modify diet, so for example, if you gave animals omega-3 fatty acids from fish, you would increase this neuroplasticity. If you gave them Western junk food type diets, you'd reduce it and it would have an impact on learning and memory in the animals. And we actually showed in 2015 that that relationship really existed in humans as well. So we had data from older adults and we looked at their hippocampal volume and their diet and all sorts of other factors, including depression, and showed that there was this very clear dose response relationship. So people who had better diets had larger hippocampi.
Dr Rupy: Okay.
Professor Felice Jacka: And that's now been shown in two further studies with much larger sample sizes. So what's true in animals is probably true in humans. But that hadn't made its way to influencing scientists to look at the link between diet and nutrition and mental health. So I set out to do that for my PhD.
Dr Rupy: So that was in 2005?
Professor Felice Jacka: Yeah, I started my PhD in 2005.
Dr Rupy: And you were specifically looking at women's health and
Professor Felice Jacka: That's right, because I was part of a big, I was in a unit that conducted a big epidemiological study and at that time they were collecting data from the female part of the sample. These were women from their 20s right through to their 90s, very representative of the Australian population. We had really good data on their, you know, diet and exercise and physical health, medical conditions, all of those sorts of things. But then we also did structured clinical psychiatric assessments on them to look at their current and past mental health. And we had a particular focus on what's called the common mental disorders, and that's depression and anxiety. And they really account for the largest burden of disability. So globally, mental disorders account for the largest burden of disability and of that, depression in particular makes up a huge chunk. It's always in the top five causes of disability.
Dr Rupy: Yeah, because I remember you mentioned that in your book, you have a whole section on the GBD, the global burden of disease and actually how, you know, traditionally we've thought to think of cardiovascular disease and stroke and dementia, all these different things, but mental health is right up there.
Professor Felice Jacka: Yeah, that's exactly right. It's the largest burden. It accounts for the largest burden because it stops people working. It stops people participating fully in life. It can really have a crippling effect, you know, on individuals, on families, on communities and certainly on society. I mean, it costs business $10 billion a year in Australia. It costs the government untold amounts of money in medical care and all those sorts of things. And what I think is really key is that if someone has depression, they're much more likely to also develop chronic disease like cardiovascular disease. And those chronic diseases in turn increase the risk of depression. So there was more reasons to think that nutrition was important because nutrition feeds into and is very important for immune function and what we call inflammation, this chronic low-grade activation of the immune system. And that was increasingly understood to be the driver of so many chronic diseases, but also depression. So I set out to investigate this in this big sample and, you know, four long years later, I did all my analyses and found that my hypotheses were pretty much supported. So women who had healthier diets were less likely to have a clinical depressive and anxiety disorders. And then separately, independently, which is a really important point, women whose diets were high in junk and processed foods were more likely. And that was of course taken into account all the things that we should consider like education and income and body weight and other health behaviours and all those sorts of things. And because it was novel and because we had very good quality questionnaires and things, that study, my PhD, ended up being published on the front cover of the American Journal of Psychiatry. And it had a big impact, but what it allowed me to do then was to go and do a lot more work in this area in a pretty short space of time because there were so many studies around the world where they'd collected data on diet and also on mental health, but they hadn't put them together. So I jumped around and did those analyses and published lots and lots of papers and yeah.
Dr Rupy: That's fantastic. Just to quickly go back to this recipe because I know there's probably a lot of people listening to what on earth is going on right now. So I've just put some half a red onion sliced into a little bit of extra virgin olive oil on a low to medium heat, added some of these sliced shiitake mushrooms, a little bit of the portobello, sauté for another couple of minutes and just gone in with the green beans as well. And that'll probably take another two or three minutes or so. And as you can tell, it's quite relaxing. It's kind of how I like to cook at home. What do you tend to eat at home?
Professor Felice Jacka: This sort of food. Yeah, yeah. I eat a lot of beans and legumes, you know, I pretty much.
Dr Rupy: Did you grow up a vegetarian?
Professor Felice Jacka: Yeah, that's right. Yeah. And I did eat a bit of meat, you know, in my younger days, but then I don't know. I don't eat, I occasionally eat a bit of meat, but not very much. And that's mainly for environmental and ethical reasons. But I also, I just love peasant food. So I just love, I love beans and vegetables and crusty bread.
Dr Rupy: It's the healthiest as well. Yeah, yeah, exactly. Yeah. And you had some interesting things to say about meat consumption as well in relationship to mental health, right? Because your hypothesis, I think initially was, you know, a vegetarian diet, plant, like plant-based probably going to be healthier than that that includes a little bit of red meat, but you came across something else, right?
Professor Felice Jacka: Yeah, that's right. So as a vegetarian, I sort of thought that people who ate meat would be worse off in terms of their mental health. But when I actually looked at the literature, I saw that there were many studies that suggested that vegetarians had worse mental health. Now, we don't know that that's a causal relationship. We don't know what's influencing what or there could be third factors that are influencing both. So you have to be really careful about that. But when I did my analyses and I looked at meat consumption, I saw this really interesting pattern of association that I just hadn't expected at all. And I looked at it in more detail and basically what I did is these, you know, roughly a thousand women, I separated them into, first of all, I took out about 20 people who said that they were vegetarians who didn't eat any meat. And then here we're just talking about red meat, not processed meat, not ham and bacon, sausages and stuff, but just lean beef and lamb. So looking at this national, the Australian dietary guidelines, it says that people should consume between three and four small palm-sized servings of unprocessed red meat a week. So we sort of divided women into those categories, those that did eat that, those that ate less than that, those that ate more than that. And then we took into account their overall diet quality because of course if people are eating for example lots of meat, they might also be eating lots of sausages and chips. Or they might be eating lots of veggies and beans.
Dr Rupy: Exactly, yeah, no two meat eaters are the same, right?
Professor Felice Jacka: That's right. So we had to sort of take that into account. And what we found was this almost perfect U-shaped relationship. So women who did consume that recommended intake of red meat were only half as likely to have a clinical depressive disorder, a clinical anxiety disorder. The pattern was there for bipolar disorder and even psychological symptoms. And it was so striking and so consistent that we went, well, you can't do a clinical trial on this. You can't take a big bunch of people and say, right, you eat meat, you don't eat meat. We're just going to follow you for the next 10 years and see if you get depressed or not. So that's why our SMILES trial, the the diet that we recommended was sort of based on a Mediterranean diet, which is this sort of food, but it did also have that red meat.
Dr Rupy: The money diet.
Professor Felice Jacka: The money med diet. Yeah. One of my PhD students is a clinical dietitian and she designed that diet.
Dr Rupy: Right, okay. Just to quickly go back to this recipe. So I've just gone in with the pre-cooked black-eyed peas. I've chopped up the toasted hazelnuts that's on the board. And we've just gone in with two teaspoons of the za'atar mix. You can get some really good za'atar blends these days. And I actually remember when I was living in Australia, because I used to live in Manly in Sydney. I was doing emergency medicine there for two years. There's like a real focus on local Aussie food. You guys are so lucky because you can grow so many different things. It's like a beautiful landscape.
Professor Felice Jacka: Yeah, yeah. You should see my backyard. I've got a veggie patch. Yeah, I just put it in in the last 12 months, I think.
Dr Rupy: Oh, amazing.
Professor Felice Jacka: So many different sorts of greens because I eat so many greens and so many herbs because I just, you know, I can go out there and grab a bunch and chuck it in. But I mean, even when I lived in apartments, I always grew herbs in pots because they're just fantastic. And so interesting how many compounds are in herbs. Like there's new ways of actually analysing plants and looking at all of the just hundreds of different compounds, even that differ from like the roots to the tips and all of those interact with all what's going on in your body and your gut microbiome and everything. So the more diversity you can get, the better. So I like to have lots and lots of greens. But I can't grow much else. I'm not much of a gardener.
Dr Rupy: No, I'm not I'm not particularly green-fingered myself and that's why I tend to stick to just like plant pots and stuff that I can grow on my plants. But it's interesting you say that about the different sort of phytochemicals that you find in herbs and spices because something I speak about quite a bit in in both my books. And on my nutritional medicine masters that I'm currently doing at the University of Surrey, the the modules on polyphenols, antioxidants, phytoprotectants are absolutely fascinating. And it resonates quite a bit with what you were talking about in your pod about, sorry, in your book about association studies, causation studies, animal studies and human trials. It's so difficult to be able to do this with a dietary intervention.
Professor Felice Jacka: So hard.
Dr Rupy: And also there's a lot of skepticism as well. You actually mentioned that when you described the SMILES trial, right?
Professor Felice Jacka: Yeah, yeah, that's right. And you know, it's justified from a purely scientific perspective. It's not when you're doing human research, particularly nutrition or lifestyle medicine research, you can't blind people to the condition they're in. We couldn't have one group that we put on a junk food diet. And then another we go. They're going to know. Yeah, yeah. This is McDonald's. You can't have a placebo, you know, if you've got an animal study, you can tightly control what they're eating, but you can't do that with humans. So you always have to be aware that, you know, there's a possibility that people's expectation of benefit was what led to the reduction. But what we saw with our trial and then with the healthy med trial, which was a larger study in a group-based setting, and that came after ours, was there was a very tight relationship between the degree to which people changed their diet and the degree to which they experienced a benefit. So people who's diet really improved, they got the most benefit from the intervention. And I think what's particularly compelling to my mind is that we did for our SMILES trial and then healthy med did it as well, very detailed economic evaluations using health economists.
Dr Rupy: I was particularly fascinated by that.
Professor Felice Jacka: I thought that was so amazing.
Dr Rupy: Because that's something I get challenged about quite a bit in clinical practice, like healthy eating is expensive. And you can understand why people might say that because when you go in the grocery aisles and you go to like the health food section, they're looking at the most expensive sorts of berries and goji berries and all this kind of stuff. But that's that's not what healthy eating is. And I was I was so pleased that you did that.
Professor Felice Jacka: Well, we did two things. We did a detailed cost analysis of the diet that we were advocating people should consume. And that's where we found that our diet that we're advocating is actually cheaper than the junk food diet that people were eating when they came into the study. But then we did an economic evaluation and what that does is it looks and it's a bit, you know, dry and nerdy, but it looks at whether if you were to adopt this, you know, at the level of the NHS or Medicare or whatever, would it be cost effective? You know, what what's the cost of delivering the diet? What's the cost of a dietitian? What's the cost and what do you get for that? What do you save? And what it showed with the SMILES trial was there was roughly a $3,000 per participant saving for those who were in the dietary condition because they lost less time out of role and they saw other health professionals less often.
Dr Rupy: That's amazing.
Professor Felice Jacka: And this just speaks to this point that if you have someone with depression and it's so incredibly common, they're at increased risk for all of these other comorbid diseases. Now there's biological reasons for that as well as behavioural reasons. If you take a diet and exercise approach to treatment, you benefit the whole person. Everything improves. And of course then they they see doctors less often. They go to the, I don't know, you know, whatever practitioner they're going to.
Dr Rupy: Absolutely. Yeah, the nurse or whether it's, you know, an allied health professional, they're feeling better. So, yeah.
Professor Felice Jacka: And this is why we think it's not just an artefact of people's expectation. The other thing too was that we found it incredibly difficult to recruit. And I think that's because people were really skeptical that this would actually help.
Dr Rupy: Yeah, you mentioned that as well, right? Like the medical fraternity were quite skeptical about this and that's why you only had about a three-year period. It was 60.
Professor Felice Jacka: 67 people, three and a half years. And it was really, really tough. But also the people with depression, I think, didn't think that it would help.
Dr Rupy: Right. Yeah. So people struggled to get people to come along.
Professor Felice Jacka: Yeah, because I remember actually reading that and I thought maybe it might have been the opposite. I would have thought if I was in their shoes, I would have wanted the diet and the counselling, but people had an expectation that the counselling was what the the treatment effect was, right?
Professor Felice Jacka: Well, possibly. So what we said to them was, look, you know, the social support, it's called a befriending protocol and it's often used in psychotherapy trials as a control condition because we know that when you go and talk to a practitioner, whoever they are, even a hairdresser, you get a benefit from just that social interaction. So you have to control for that because that's what you get when you see a dietitian. But it also is beneficial in its own way. But people, I think who did come into the trial were much more willing to be in the dietary group. So that's a problem. So what we really need is studies where you have two different dietary interventions that people are happy to go into either one. And that's tricky because there's nothing to say that one form of a healthy diet is any better than another form of a healthy diet. So it's it's very challenging from a methodological perspective. But the fact that people experienced so much benefit and that there was such a tight link between how much they changed their diet and how much they improved, suggests to me that there's something really powerful in this.
Dr Rupy: Absolutely. And we're not talking about, you know, mild depression, even though that's very important.
Professor Felice Jacka: No, moderate to quite severe.
Dr Rupy: Moderate to severe. And then some people, some of the patients that you mentioned went into remission as well.
Professor Felice Jacka: Well, more than 30% of those in the dietary group went into remission compared to about 8% in the social support condition. And what's really great is that we get a lot of participants from SMILES contacting us years later. And they say, look, it just changed my life.
Dr Rupy: Felice, how was your lunch?
Professor Felice Jacka: It was so delicious. It's my perfect meal.
Dr Rupy: Good, good. I mean, we've talked quite a bit about your book already and, you know, all the different topics. One of the things that we we didn't mention was exactly what the SMILES trial was. So would you mind just telling us a little bit briefly about what that what that trial entails?
Professor Felice Jacka: Sure. And also just the the reason that we did it. So, you know, I discussed my PhD as being the study, the first study to look at the link between diet quality and mental health in, and then we went on and we did a lot more research in different age groups and different countries and different cultures. And of course, other people were also doing research. And so by sort of 2012, we had this really quite robust evidence base linking the two things. But you can't assume that correlation is the same as causation. You know, and with these epidemiological studies, you're limited in knowing whether one thing is actually causing another. So you need to do randomized control trials or you need to do interventions, experiments. And so we wanted to try and answer that $64 million question that people would ask us, you know, I'm depressed, should I change my diet? And we didn't have any evidence one way or another that that would be a useful strategy. So me being really naive and, you know, fresh out of my PhD, I went, I can design a randomized control trial. And managed after a couple of years to get the funding for it, although they cut the budget by 36%. So we were doing everything on the smell of an oily rag. It was really, really challenging.
Dr Rupy: Why did they cut the funding? What was the
Professor Felice Jacka: Oh, that's just what the National Health and Medical Research does. So, but, you know, we limped along and we managed to to do this trial. It took three and a half years to recruit everyone. It was very slow. But basically what we did was we recruited people to who had moderate to severe clinical depression, which is of course really common, very, very disabling. And we randomly assigned them to receive either social support, which we already know is really helpful for people with depression, or dietetic support, so nutritional support with a clinical dietitian. And so for three months, people came in either weekly or fortnightly and saw either a research assistant to do the social support thing or a clinical dietitian. And the dietitian worked with each participant in the dietary group to help them to make positive changes to their diet in a way that was achievable, feasible, you know, not too challenging. And so, you know, to increase the amount of vegetables and fruits, to increase the diversity of plant foods, different types of beans and legumes, and often people hadn't even eaten legumes to start with. Getting people eating nuts and seeds.
Dr Rupy: They don't know what it is, you know, like now when I mention the word legumes, people kind of look at me funny, like, oh no, like, you know, beans, chickpeas, lentils, mung beans, all that kind of stuff.
Professor Felice Jacka: Yeah, yeah, peasant food. But also at the same time, of course, to reduce the the junk and processed foods, to reduce the sweets and the fried foods and the packaged foods and those sorts of things and soft drinks. And so over a three-month period, people were supported to do that. And then at the end, we looked to see how everyone was doing in terms of their depression scores and we found a really profound difference between the groups. And as I noted, you know, the more people change their diet, the better off they were and it was it was quite a stunning finding. We didn't expect to see a big difference between the groups because we had a quite a small sample size. But then a few months later, another group in South Australia did a very similar thing but in a larger study in a group-based setting. And where they helped people to learn how to cook and how to shop and, you know, how and eating together and all the rest of it. And the the comparison group was a social group and they were really popular, you know, they're off to the movies and playing games and doing all sorts of fun things. So both groups, the people really enjoyed it. But again, we showed or they showed that there was a much greater improvement in depression in those who got the dietary support and who changed their diets.
Dr Rupy: Yeah. I mean, that's I mean it's phenomenal. I remember hearing about it because it was literally everywhere. It was like all plastered all over the newspapers. You got some amazing coverage. Was that just purely out of, you know, it growing virally or did did you make a concerted effort to put it out there?
Professor Felice Jacka: I I I write a pretty mean press release. Not blowing your own horn or anything. I was so, you know, we were kind of so stunned by the findings and just the the size of the difference and, you know, there just was something in the air. We knew that there was a real appetite for this. A lot of the work that I've done because I've led so many of, you know, the first studies in adults and in children, adolescents, the first study looking at brain plasticity. It often gets a lot of media. And to my mind, if you want, you know, knowledge to be transmitted through the community very quickly, you can't wait for governments to write, you know, public health messages or you have to get it out there. And to me, always the context is that because of the the massive changes to our global food environment and because of the activity of big food, poor diet is now the leading cause of early death in men and number two in women across the globe. So the way our diets have changed is just so terrible and it's having such an impact on people's health. And at the same time, mental disorders account for the leading global burden of disability. So the fact that the two things are linked is really important and I wanted to get that message out there. So, but I even I was pretty amazed at the impact that it had and, you know, we ended up in the Wall Street Journal and NBC and CNN, like just all over the news. And it continues. I mean, that was 2017 and now in 2019, we're still, you know, turning up in articles, the New York Times just a couple of weeks ago. I mean, you know, it continues to reverberate, which is great.
Dr Rupy: One of the things that I really love about your book is the bravery by which you confidently talk about your own personal experiences with mental health, both your your daughter and your your personal experience. And that kind of ties in with that maternal and paternal responsibility for mental health or health during conception. I find that topic absolutely fascinating. Would you mind just going into a little bit more depth about that?
Professor Felice Jacka: Yeah, so, you know, like many, many, many people, I had a long history of what we call common mental disorder. So anxiety disorder probably manifested in childhood. That's when they often do. And then by early adolescence, I was starting to experience panic attacks, but also then clinical depression and I had many episodes throughout my adolescence and really quite severe. Now, of course, that's not uncommon and I had a very strong family history. My father had had very severe major depression with psychosis, so had both of his parents. So the genetics were playing a really big role there as well. And, you know, I'm very open about this because I don't see why we should not be talking about mental health in the same way we'd be talking about a physical health condition. And similarly with treatment, you know, reducing stigma. But when my first daughter, when I was pregnant with my first daughter, normally I'd eat a pretty healthy diet, but I had just such severe, awful morning sickness. It was like having this massive hangover. And I just couldn't even look at a vegetable and I ate, you know, all the wrong things for that first few weeks.
Dr Rupy: One of my best friends is actually going through that at the moment and she's a massive healthy eater and she can't look at broccoli.
Professor Felice Jacka: No, no. She just can't.
Dr Rupy: I know, it's really weird. It's like, oh, you want is chips and ice cream. That's literally her diet.
Professor Felice Jacka: Oh, I know. So and but also, of course, I was really anxious, you know, first time parent and there were lots of reasons why my eldest daughter might have been born being quite anxious herself. And we have no idea whether the food had any input into it, but certainly she experienced a somewhat similar trajectory to me in that she certainly developed panic disorder when her early teens and some depression, not nearly as bad as mine, thank goodness. But we just don't know whether, you know, what I did or didn't do in pregnancy plays a role in that. But the point I make in the book, and I think this is critical, is that all of us as parents have enough things to feel guilty about and we're doing the best that we can. And the key thing is that the environment needs to support healthy choices. So if you go out every single day and all you see is junk food purveyors and you go and fill up your car with petrol and all you see is soft drinks and packaged food and and sweets and things like that and and these foods are so heavily marketed, they are everywhere and we are designed as humans to want those high energy foods and they interact with the reward systems in the brain. And then of course, people have kind of forgotten how to cook and we're busy and all sorts of reasons why we may choose the wrong foods. And this is where the food environment has to change to make healthy eating the easiest, the cheapest, the most socially acceptable, the most heavily marketed. And, you know, teaching people the basics of cooking again.
Dr Rupy: Yeah, and you talk actually about junk food and its impact particularly on adolescent brains as well and how they may have less ability to say no to these things because of the impact on their reward system.
Professor Felice Jacka: That's right.
Dr Rupy: What is, so what is your sort of idea for how we can actually improve adolescent health through food? Because at the moment, particularly in this country, I'm not sure if it's the same in Australia, but chicken shops, fast food takeaways, all the major sort of junk food brands, they surround schools. They literally like if you look at a map, you can see that they're populated around schools. They're directly targeting, whether it's intentional or not, that's where they are. How are we going to get around that?
Professor Felice Jacka: It makes me furious. I think we just, the first instance, and I can really only talking talk about Australia and not other jurisdictions because I don't know what the planning laws are like. But in Australia, local communities don't have the power to say no to that because the planning laws happen at the state level. So we need to give communities and schools the power to say, no, we don't want that in close proximity. Uber Eats is becoming a really big issue because then it actually doesn't matter where the things are. They can come anywhere. But, you know, in Australia, so around the world, as I said, poor diet, the leading cause of early death, responsible for by 2030, according to the WHO, at least $30 trillion worth of health costs, and that's without factoring in all the mental health and, you know, things like dementia and those sorts of things. And yet, governments have done almost nothing to change the status quo because big food is so powerful and their ability to lobby and the money behind them is just massive. But in Australia, there's at least the beginning of a discussion about adopting a whole lot of public health policy recommendations from the people working particularly in obesity prevention. Now, to my mind, sometimes it's problematic if you make the whole conversation about obesity. Because there's a few reasons for that. One is that once you've put on weight, it's very, very difficult to get it off and keep it off. So people often give up if they think that the only reason they have to eat healthily is to avoid being fat and they are fat anyway, they go, well, I might as well just eat the burgers.
Dr Rupy: And there's a physiological reason behind that as well because your body will defend that weight set point because it feels as if it's going into starvation mode. And so that's why it upregulates your your satiety levels and it will continue to get more hungry.
Professor Felice Jacka: Yeah, and, you know, you put somebody with obesity in an MRI scanner and show them pictures of food and their brain lights up like a Christmas tree. Interestingly, that's lost almost immediately after bariatric surgery. I think that's very, very interesting. Yeah, and they don't know why or how that works. But the other thing about obesity, certainly in relation to mental and brain health, is that that relationship between diet quality and mental health in all of the research we've done is quite independent of obesity. It's quite independent of body weight. Now, we know that depression prompts weight gain. We know that being overweight can increase the risk of depression, probably through inflammation. But the relationship that we see is independent of that. In the SMILES trial, just as an example, the average BMI was about 30 and that didn't change. No one changed their weight because of the diet.
Dr Rupy: What time period was the SMILES trial again?
Professor Felice Jacka: Over a three-month period. So people didn't and it wasn't a weight loss diet. But it was about improving the quality of your diet. And I think that's a really powerful message is that don't worry about your weight. That'll take care of itself because if you start feeding your gut and feeding your self, your brain with good food, you'll start to feel better. You'll start to naturally regulate the amount of food that's going in. You'll start to want to do more exercise and all of these good things will flow. And if you lose a bit of weight, fantastic, but if not, don't worry about it because you are doing the very best thing for your long-term health.
Dr Rupy: Yeah, that's music to my ears. I mean, in my first book, I remember the the paragraph that I wrote about how healthy eating and what you should be striving for is independent of weight loss. If you go for weight loss, you're looking, you're not looking at the whole picture. If you're just trying to adopt healthy habits and behaviors, you'll be you'll be surprised at all the other healthy aspects of of wellness that will come to you. One of the things that you talk about in your book is some sort of like fad diets and supplementation and that kind of stuff. One thing that really stood out to me was the suggestion in the literature that a keto diet might be suitable or may have some benefits for schizophrenia. So a keto diet, just for those who are listening, is one where you have predominantly fats in your diet or you you consume a lot of your energy and your calories from fats rather than carbohydrates or protein. It's a very extreme diet. It's very restrictive. There are some clinical applications for epilepsy. But I wanted to get your understanding of what potentially could be the mechanism behind why it might be useful for schizophrenia and whether that's purely because of better metabolic control and glycemic control that we can achieve perhaps through some other less extreme measures.
Professor Felice Jacka: Yeah, yeah. I have to say I'm not a fan of the ketogenic diet. It's enormously concerning to me that it's promoted so heavily by so many diet gurus on the basis of extremely scanty cherry-picked evidence. And, you know, really when you drill right down, it's because people think that they can lose weight and it's very heavily promoted by the bodybuilders and, you know, people who are very fixated on their appearance. Based on everything we know about the gut, it would be really bad for the gut because the gut and does not like high fat and the gut really doesn't like low fiber and that's what a ketogenic diet is. However, there are some clinical applications. So in epilepsy, there's a quite a large proportion of people with treatment resistant epilepsy that will respond to a ketogenic diet. It's an incredibly strict diet. It's a really awful diet and people struggle to stay on it long term and it can have a lot of negative health impacts and they know that from people with epilepsy. But colleagues of ours have done a lot of animal research and they think that it may be of use in psychosis, like we're talking about quite a serious mental disorder. And there's been a few case studies of people with psychosis who have been put on a ketogenic diet and have had a, you know, reduction in their symptoms. Now, because this happened in the states, we don't know if that's just because they stopped feeding them junk food or, you know, like there's a whole lot of reasons why that might have happened. But one thing we do know about psychosis and schizophrenia is that many people with those conditions have inbuilt problems with glucose metabolism. They're not, you know, they don't deal with glucose in the same way that someone without that condition does. So we're hoping to generate some empirical data on this. So the study and it's going to start in the next couple of months will be conducted in an inpatient unit in Finland. And the reason it's going to be in Finland is because in this hospital, they already have patients with epilepsy who are in there for treatment and so the hospital menu has the ketogenic diet as a, you know, part of its protocol. Yeah. And then also these young people with schizophrenia, psychosis, they're in there for a period of time. They can't get out and there's no cafeteria. And I'm told there's no Uber Eats that just doesn't happen. So basically it's almost the only way that we're ever going to be actually able to test this. I'm very interested, but even if we do see that there's a possible benefit to people's psychotic symptoms, again, we don't know if that's because we've removed things from the diet that they may be reacting badly to. We're very interested in the possible role of food sensitivities in people with psychosis. We think maybe a small proportion of people have because of, and this goes right back to the gut, some fundamental issues with the gut that could go right back to the start of life that they don't deal as well with a whole lot of different dietary inputs. So removing potential food allergens from their diet may also have a benefit. So we want to test that as well. But what we are doing, and I think this is going to be really, really interesting, is we're doing a very detailed investigation of the impact of the on the gut of a ketogenic diet. Now, this is our modified keto diet that has less saturated fat, more mono and polyunsaturated fat, avocados and nuts and fish and that sort of thing. But it's still a really strict ketogenic diet. And we're going to take lots of poo samples and lots of blood samples from about 10 people and really track that in great detail over a month to see what happens to the gut because based on everything we know, it's going to be really nasty for the gut and anything that's bad for the gut is going to be bad for you. But there may be adaptation, we don't know.
Dr Rupy: Yeah, yeah. And I've I've heard of some adaptations looking at a healthier keto diet, not that I think there is a healthier version. But I've come across some studies that a keto diet is the equivalent of having a round of antibiotics in terms of what it does to your microbiota. So that's something to always bear in mind.
Professor Felice Jacka: Oh, look, and I just came across a new study and I don't know how I missed it because it was published a few months ago now, but it was published in Oslo. It's a really important study. When you look at the ketogenic diet and the the health, you know, what people are purporting it does to to reduce blood glucose and all of those sorts of things. We really don't know whether that's just because people have lost weight and you get a lot of these health benefits in the short term when you lose weight. This study in Oslo, it took more than 30 young adults, healthy adults in the healthy weight range. So they were really healthy, they were nice and slim, doing all the right things and they put them on a keto diet for three weeks. Now, what happened to their blood lipids is just extraordinary, particularly because there was such pronounced variation. So they all got exactly the same food, but LDL cholesterol increased between 5% up to 107%. So in some people, it just went off the scale. Even more concerning, there were two really quite serious adverse events, cardiomyopathy.
Dr Rupy: Okay, yeah, yeah.
Professor Felice Jacka: And then an autoimmune thyroiditis.
Dr Rupy: Wow. Is that right how you say it? Yeah, autoimmune thyroiditis. Yeah.
Professor Felice Jacka: Two young healthy people within three weeks. In fact, that happened really quickly within a week or so.
Dr Rupy: You can almost understand why that might happen as well because if you're giving an insult to your gut microbiota and that's inherently involved in your immune regulation and you have a patient that has a propensity toward autoimmune disease because of a genetic predisposition, then you're essentially lighting the fire with a keto diet.
Professor Felice Jacka: That's right. And it just blows my mind that people are advocating this as a sort of diet that cures cancer and, you know, the whole works. It's it's really, I think, unethical because at this point, we do not have the data to say that this is a safe thing. Some people may respond really well to it, but others are not going to respond well. And what this study showed was that some people experienced a really massive increase in their LDL cholesterol, which we know is a profound risk factor for heart problems, no matter what the the conspiracy theorists and the diet gurus say.
Dr Rupy: There's so many things that I wanted to chat to you about regarding the immune system and meta-inflammation. We touched on inflammation earlier when we were cooking. But I think you've got a really nice analogy for explaining what inflammation is and what meta-inflammation or low-grade chronic inflammation is and how that relates to to mental health.
Professor Felice Jacka: Yeah, well, I mean, based on what we know, and I'm not an immunologist, you know, if you if you have an injury or a severe virus, your immune system springs into action and the little messengers that are part of that whole immune response, these proteins are called cytokines. And I mean, there's a whole lot of different ones. And basically, they run around and make sure that things happen and that you get healed, hopefully, if your immune system is working well. But what you don't want is this those cytokines hanging around over the long term. But what we know is that there are a lot of things in our Western life that really prompt this low-grade inflammation, this systemic inflammation where these cytokines, it's like your immune system is on low-grade alert all the time. And they're things like not having enough sleep and sedentary behaviors and smoking and lack of vitamin D and stress and all of these things. But of course, diet is a really big part of it. We know that a healthy diet that's high in plant foods and whole grains, etc, prompts a reduction in inflammation and we know Western diets increase inflammation. But of course, inflammation doesn't just happen in your body, it happens in your brain as well.
Dr Rupy: Well, this is a relatively new recognition, right? That inflammation and the cytokines can cross the blood-brain barrier.
Professor Felice Jacka: Yeah, yeah. And I'm not an immunologist, so I don't want to go into too much detail there, but there's all sorts of new knowledge coming out of the field that I think's really interesting. But basically, you know, the driver of all of this, so we know about the immune system and its role in prompting depression. And we know this from a whole number of different studies and different ways of coming at the research. And we know that brain plasticity is involved in mental health and that diet influences mental health. But what we now know is that the gut and the microbiota that live in the gut play a key role in all of those things. So they're very, it's very important, it's like the heart of your immune system, your gut. It also influences the health of your brain, the integrity of your blood-brain barrier, your brain plasticity, all of these things, as well as your body weight and your metabolism, etc. Now, it's a very new area and it has to be said that most of what we know comes from animal studies. So we have to be careful in extrapolating too much. And we're also really struggling with the methodologies. You know, like, what does this mean? Just because there's a bacteria in there, like, what is that good? Is it bad? And then we're finding out that bacteria can do all sorts of different things and sometimes they can be baddies or goodies depending on who else is in the zoo and, you know, how they're working together. So it's horribly complicated. But there are some basics that we're pretty sure about. And the first thing is that the gut bacteria, their primary role is to break down dietary fiber. So the dietary fiber that your human enzymes can't break down, that's their job. And they break down the dietary fiber. So that's in the things like the beans and legumes and plant foods and all the stuff that you've just seen. And when they do that, they produce a whole range of what are called metabolites, many, many different ones. And we're only just starting to figure out about some of them. The short-chain fatty acids have been looked at quite extensively. Short-chain fatty acids interact with pretty much every cell in your body through these G-protein coupled receptors and they influence how your genes behave. They are very important in the immune system and the health of your gut lining. It should have a nice thick mucosal layer. That's really important in having good immune health. There's many things that can break down that layer and then you get this what's called metabolic endotoxemia where you get these pro-inflammatory things getting out of the gut and into the bloodstream. But the gut bacteria do so many things. They synthesize vitamins, they synthesize neurotransmitters, they also prompt the synthesis of neurotransmitters. Now we don't know that those neurotransmitters actually get into the brain. We do know that more than 90% of serotonin is actually produced in the gut, but it may not cross the blood-brain barrier. But those neurotransmitters do signal to the brain via the vagus nerve, the gut-brain axis. But the bacteria also control how much serotonin is produced by the metabolism of tryptophan and they're in charge of that. So there's a whole lot of different ways by which we think the gut bacteria interact with the brain and behavior and we're just starting to really do the studies in humans to try and unpick all of that. But it's very new.
Dr Rupy: Yeah, absolutely. And I think a lot of people kind of jump the gun with a few things that you probably mentioned, right? So tryptophan, specific types of dietary fibers and a lot of spin-off supplementation sort of practices have come about. You were just telling me before the pod about how you were just at a recent conference and you came across some really interesting research looking at which supplements or nutraceuticals may have benefit and which don't. And you were saying it's pretty pretty thin evidence.
Professor Felice Jacka: Pretty thin evidence. So, colleagues of mine have done just recently a mega analysis, which is like a meta-analysis of all the meta-analyses. So it's basically brings together everything we know from randomized control trials about the impact of supplements, nutritional supplements in psychiatry. And pretty much the evidence is pretty limited. EPA, which is part of the long-chain omega-3 fatty acids, like fish oil, seems to be helpful for people with clinical depression if they have high levels of inflammation, which is about half of people with clinical depression. So EPA, yes, tick, but again, short-term, it's not long-term, short-term. Methylfolate, it's a form of folate, that has some pretty good evidence. And again, it's during the acute phase. It's when people are depressed. And what happens, of course, when you have many different sorts of medical conditions, but including depression, your immune system is activated. So you have more inflammation. And what that inflammation does is it kind of burns up your nutrients in a way. You get this sequestration of nutrients and you you your nutrient levels drop and you also get oxidative stress and that interferes with the long-chain omega-3 fatty acids in the brain cells because they make up an important part of the brain of the neuronal wall. So that's why I think the EPA seems to be useful because it can bring that back and same with the folate. There's some evidence for something called NAC, N-acetylcysteine, which is a precursor.
Dr Rupy: We use it in emergency medicine.
Professor Felice Jacka: Yeah, that's exactly right. And it's great for that in a short term, but it's not something that I would be taking long-term. And this is the thing, when you take a supplement, you're not taking it with all the other cofactors and things that you should be consuming. I don't take supplements. I don't actually trust them. Ever since I found out that antioxidant supplements, so vitamin C or vitamin E, you take them before exercise and you lose a whole lot of the benefits of exercise because it interferes with this whole really complex processes.
Dr Rupy: Yeah, I remember coming across that actually because vitamin C, particularly amongst the sort of physio or the personal training community, has been thought of like a no-brainer after exercise because it's anti-inflammatory. But what you're doing is blunting the benefits of exercise, which lead to ultimately shearing of your muscles and inflammation. And it's that it's that little bit of low-grade inflammation that actually leads to resilience of the body over time. It's almost like the plant hormetic effect. I'm fascinated by this theory of like, you know, a little bit of bad is good for you in the long run. So that's interesting. So no vitamin C or vitamin E.
Professor Felice Jacka: I don't. I mean, I'll take a bit of vitamin D in winter time, but I do try and get it from the sun if I can. And I'm Australian, so I get to do that.
Dr Rupy: We have we have recommendations to take vitamin D3 now in the winter months, but as you've experienced, our summer in June is not always sunny over here. So, yeah. I think vitamin D is pretty pretty important for for people in the UK. But yeah.
Professor Felice Jacka: Yeah, yeah. But that's about the only thing that I take. I just don't, I've never taken supplements. Probiotics, you know, there's the evidence is pretty mixed and I would much rather be getting fermented foods into me. And I think fermented foods is really interesting because they've been part of traditional diets forever. There's a lot of misunderstandings about fermented foods. So say if you took kombucha, for example, fermented tea and people will say, oh, but all the bacteria are dead because they've eaten all of the the sugar substrate, they've and now they've died off because they don't have anything else to eat. So there's no point taking it. Well, actually, that's not how it works. So what happens is during the fermentation process, those bacteria are producing all of these metabolites, so many, they're called biogenics and they are they're multitudinous and we don't even know what most of them do. But we also know that the bacteria can still have bioactive effects even if they're dead. So I think fermented foods are great for a whole range of reasons. We're really keen to test them in clinical trials and that's something we're working on at the moment. And also they're just delicious. I just love, I make my own kefir.
Dr Rupy: Oh, you have your own like, so you make your own kefir at home with the grains?
Professor Felice Jacka: Yeah, yeah, with the grains. So simple, so cheap and just so tasty. And then I make smoothies with the kefir. I love it. My husband not so keen. I'll get him there.
Dr Rupy: I've heard of this term banded around actually called psychobiotics, which are probiotics that potentially have the impact or can have the impact on on mood. But I think you're right, it's a fascinating area of research, very, very much in its infancy at the moment. So at the moment it's just probiotic foods.
Professor Felice Jacka: Yeah, and there is some really interesting data though. There was a fantastic study Bob Yoken's group published probably about six months ago where they they took and this is to me the most compelling study so far in psychiatry. Patients with bipolar disorder, like serious bipolar disorder, who had been hospitalized with mania, when they came out of hospital, they were randomly assigned to get either probiotics or placebo. And then they were followed over time to see how long it would take for them to go back into hospital with mania. And there was a really big difference. The ones on the probiotics took a lot longer to go back into hospital.
Dr Rupy: Gotcha.
Professor Felice Jacka: So that's very cool. But the psychobiotics, so Professor John Cryan and Ted Dinan from Ireland, right? Great buddies of mine and they're really the world experts, you know, and they've got a great book called Psychobiotics, which is all about this. But they would say, look, at 99% of the bacteria strains that they've tested in animal models don't do diddly squat. But there are some that are and I do think that there's probably huge potential there. It's just that we're not there yet and going and getting some probiotics off the shelf and consuming them is probably not particularly worthwhile unless maybe you've if you've had antibiotics, it's certainly not going to hurt.
Dr Rupy: Exactly.
Professor Felice Jacka: But I would be getting the kefir and the kombucha and the tempeh and the sauerkraut and everything else into me.
Dr Rupy: It's something I actually tell patients whenever I give antibiotics. So look, there's no evidence behind a probiotic supplement. It's unlikely to do any harm. I'd prefer you get it from probiotic foods, but we're just not there yet. And there's so many different variations as well, right? I mean, depending on your genetics, your current state of your microbiota, whether you're dysbiotic or not. It's it's almost like the keto diet for some people, it's great. For other people, absolutely deadly. And potentiates in some cases autoimmune conditions, which you talk about in your book as well, which I was I was quite pleased to to read about. And also, there was a study that you you mentioned, it was something that I I wrote an essay on recently. I think it was O'Keefe and colleagues and they did a crossover study where they took people who were still living in Africa, in South Africa, I think it was.
Professor Felice Jacka: Oh, it's one of my favorite studies.
Dr Rupy: It's a fantastic study. Yeah.
Professor Felice Jacka: It's amazing.
Dr Rupy: And then they crossed over the diet with people of African origin who were living in America and therefore eating a Western diet. And they crossed them over for two weeks and they found profound changes, right?
Professor Felice Jacka: Yeah, that's right. So, you know, we know that people who are living more traditional lifestyles have a much healthier gut microbiome, more diversity, more short-chain fatty acids, all of the stuff. And they compared South Africans living a rural traditional lifestyle to African Americans having the sad, the standard American diet. And of course, their gut looked really kind of awful and had higher levels of inflammation and these markers that we know are risk factors for bowel cancer. But that was the cool thing. They swapped their diets for two weeks and the poor rural South Africans, their, you know, their gut health went down the toilet, so to speak, and the inflammatory markers went up. But it got better in the African Americans. That's so powerful. That's saying in two weeks, you can have profound changes on your in your health by just changing what you're feeding your gut microbes.
Dr Rupy: Absolutely. Yeah. It's incredible that. And so to to summarize, I don't because there's so much information packed in your book. I mean, you talk about dairy, gluten, specific diets, you even put the details of the money diet that you put in that you used in the SMILES trial. If we were to categorize what things that we need to be doing for mental health, what sort of things? So we talked about whole grains and and fiber, which we we had in our lunch today. What other things are you looking at? And fatty fatty fish supplements or potential supplements?
Professor Felice Jacka: Look, I think it's really important to understand that you don't have to get this perfectly right. And, you know, I go very much for the 80/20 rule. In Australia, average, like teenagers are having on average seven serves of junk food a day. Seven serves. Less than half a percent of Australian children and adolescents are getting the recommended intake of veggies and legumes. Less than 5% of adults. In America, something like 60% of their average energy intake is coming from ultra-processed foods. So this is not just a problem of people who are poor and uneducated. It is a massive and on a global scale. So if you moved your diet to be 80% pretty good, you know, you would be doing so much better than the vast majority of the population. And then that still allows for, you know, I love ice cream. Friday night, ice cream time. You know, I like chocolate. You know, I'm not super, super strict and it's not prescriptive.
Dr Rupy: You got to give your ice cream recommendation for Melbourne. I know Melbourne's like a hot bed for new restaurants.
Professor Felice Jacka: Yeah, yeah, Messina.
Dr Rupy: Messina. Yes, so we have a Messina, a bunch of Messinas in Sydney. Did it originate in Melbourne or Sydney?
Professor Felice Jacka: No, actually. Not sure. But I also love, oh, yeah, no, there's many, especially around Carlton, the Italian areas, so much good gelato. I know, I love ice cream.
Dr Rupy: Okay.
Professor Felice Jacka: So, you know, 80% of your your diet, you're just going for whole foods and it doesn't have to be that difficult or complicated, you know, porridge for breakfast. Yay. You know, a bit of Greek yogurt with some oats on top and whatever. Yay. Lunch like we had today, just, you know, good quality sourdough bread, whatever. The sorts of recommendations we gave in the SMILES trial were so simple. They were like a, you know, Ryvita type biscuit and a tin of tuna and some sliced salad. Bang it on. That's it's cheap, it's easy, it's quick.
Dr Rupy: And for that simple diet to have that dramatic effect over three months.
Professor Felice Jacka: It's just extraordinary. So you introduce fiber. Fiber is key. That is number one. Polyphenols, you know, coming in all the colorful fruits and vegetables. They seem to be really powerful. There's some really interesting studies showing that if you get rodents and you put half of them on a high fat diet and the rest on a normal diet, the ones who are getting the high fat diet, of course, they get really fat and they put on lots of weight. But if you take a third group and you give them that high fat diet, but you also give them polyphenols in the form of, you know, blueberry supplementation or whatever, they only put on half as much weight.
Dr Rupy: Wow.
Professor Felice Jacka: So it's the only thing that's different and it mitigates weight gain. So you've got to look after your gut. Your gut and I think that makes it easier for people. They get told that they should eat their fruits and veggies, but they don't really know why and they think, oh, well, maybe one day I'll have a heart attack, but that's off in the future. But if you say, and a lot of people reduce like the berries, for example, just to its polyphenolic components, so the flavanols and stuff like that. But actually, you know, it's the fiber, it's the other parts.
Professor Felice Jacka: All the other things that we haven't even started to measure yet. This is what's so powerful about plants. But just this knowledge that if you feed your gut, you're going to be doing good and you don't need to know the detail of which bacterial strain is doing what. You just need to know that your gut bugs need fiber to do what they do. If you don't have enough fiber, they can't do what they do. You just need to know that lots of different types of fiber and different types of plant food help lots of different types of bugs to live there. It's like a zoo. You want this real biodiversity in your gut. My husband and I have just written a kids' book.
Dr Rupy: Oh, have you? Another book.
Professor Felice Jacka: Yeah, and it's called, it's called There's a Zoo in My Poo. And the idea is that we want to get kids actually going, I'm the zookeeper. I'm in charge of these guys. I've got to look after them. And that means I've got to feed them the right things. And I think that's true for adults as well. That it's making it very concrete like that is going to be really powerful.
Dr Rupy: That's brilliant. I can't wait to read that.
Professor Felice Jacka: Yeah, yeah, it's quite hilarious.
Dr Rupy: It'll help parents, I think, as well, think about it.
Professor Felice Jacka: Totally. I know. And and it's full of illustrations because my husband's a crazy illustrator. But it's also full of, you know, poos and bums and farts and mucus and all the things that kids love. So we had a lot of fun doing that together.
Dr Rupy: That's great. I can't wait to read it.
Professor Felice Jacka: Yeah, it's funny. But I think that idea that this is something very concrete, it's about your gut, you can change it really fast. You just need to make those switches to your diet. That is so powerful.