Elizabeth: What I also think is exciting is that working in cancer over many years, it was always like, yeah all of this is important in prevention, but it's not important in treatment and you should just go away and have double cream and digestive biscuits. And I think what's really exciting with the work that Valter's doing is you know making it part of an integrative approach, a treatment during cancer treatments. And for me the really interesting thing is survival because you know maybe not just this element but other elements that people can take on could we really start to turn things round, not just for cancer but for other long term conditions as well.
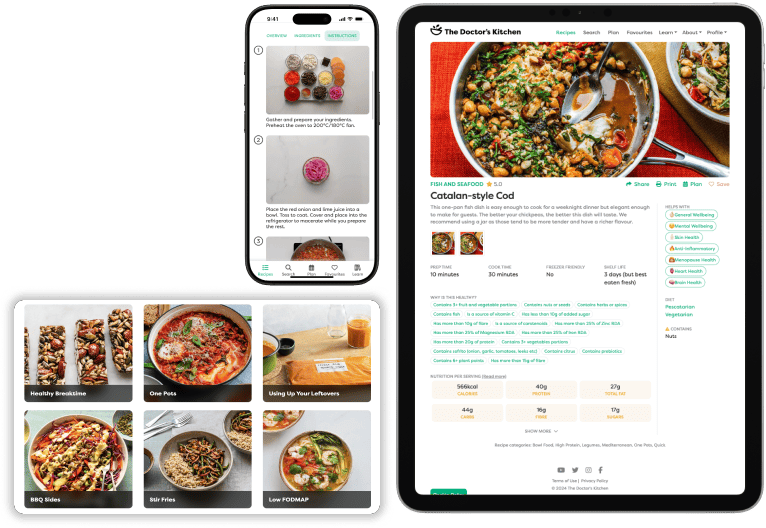
Dr Rupy: Welcome to the Doctor's Kitchen podcast. The show about food, lifestyle, medicine and how to improve your health today. I'm Dr Rupy, your host. I'm a medical doctor, I study nutrition and I'm a firm believer in the power of food and lifestyle as medicine. Join me and my expert guests where we discuss the multiple determinants of what allows you to lead your best life. Fasting as a tool for health is becoming a popular question whenever I do live talks and the interest in fasting is absolutely huge. We've done a dive into fasting with previous guests on the podcast, just check them out on the doctorskitchen.com/podcast. And today I'm talking again with Professor Valter Longo and Dr Elizabeth Thompson about fasting as a tool in diabetes and even to support cancer patients during chemotherapy. We've had Professor Longo on the pod before introducing what fasting means and how it works. So if you want a more specific explanation into fasting mimicking diets, also known as FMD that we'll refer to quite a bit in this podcast episode, make sure you listen to that episode first. We also dive into Dr Thompson's own experience with fasting, the new data from Valter's lab as well as other labs and also since we've last spoke, the long term effects, drawbacks and implementation and why it needs to be standardized. Remember, fasting is still an emerging therapeutic tool, so please exercise caution when trying any of these techniques and if possible, do it with the guidance of a practitioner. Dr Elizabeth Thompson is a very experienced medical doctor having trained in medicine at Oxford University and completed her clinical training at Guy's Hospital in London. She's also the chief executive of the National Centre for Integrated Medicine and an experienced medical homeopath specializing in women's health including the menopause and supporting the health and well being of cancer patients. Dr Valter Longo is professor of gerontology and biological sciences and director of the Longevity Institute at the University of Southern California, one of the leading centres for research on aging and age related diseases. The Longo laboratory published key findings on the five day periodic dietary intervention called fasting mimicking diet, FMD, and showed in randomized control trials that FMD reduces the risk factors and markers associated with aging and diseases. Dr Longo's most recent studies focus on the use of FMD to activate stem cell based regeneration to promote longevity. Today we talk about Dr Elizabeth Thompson's personal experience with fasting, the recent findings on periodic fasting in cancer, why fasting needs to be standardized, the drawbacks of fasting and why it isn't a miracle cure, the long term effects of periodic fasting and why the implementation of fasting may be easier than you think. We also have a chat about protein and longevity. Dr Elizabeth was in the middle of conference chairing, so she had to leave halfway through, but me and Valter have a prolonged conversation about other stuff while she's not there. Remember, you can download the Doctor's Kitchen app for free to get access to all of our recipes with a 14 day free trial. Android users, I am working very hard on it. And do check out the eat, listen, read newsletter that you can subscribe to on the website at the doctorskitchen.com where I give you something to eat, something to listen to, something to read every single week to help you have a healthier, happier day and week and month. On to the podcast. Elizabeth, Valter, fantastic to have you both here. I know it's a busy conference, so we're going to do this kind of rapid fire, but I do want to dive into some some incredible topics. First of all, why don't we talk about the conference that we're currently at at the moment. Elizabeth, tell us about integrated medicine and the purpose of this personalized medicine conference that you've run.
Elizabeth: Well, we're pretty excited. We were planning it pre-pandemic, but we didn't know we were going to have a pandemic. Now to have over a thousand attendees per day to really look at integrative and personalized medicine. It's it's exciting because it really is starting to feel like a movement for change. How do we get this broader, more compassionate model that has wellness right at the heart? And today I felt for the first time like we wouldn't be that far away before systems can change, we can look after doctors, nurses, healthcare professionals, give them time, because we need time to really work with individuals. But also this range of approaches that science is now really helping us with. So things, you know, even in that last session, so leaky gut, crazy idea 10 years ago, loopy. Now with COVID-19, we start to really understand some of these factors that might play a part, what's happening with chronic fatigue. So I just feel like science is emerging really fast and this integrative medicine model is there at the right time, at the right place. And this conference, I think proves it. Look how many people are here, how many organizations, everyone wants to be part of it.
Dr Rupy: Yeah, absolutely. And I think it's interesting you say that about how these previous ideas were thought of as fringe and now they're becoming mainstream. Valter, you've been on the podcast before talking about fasting mimicking diet and fasting in general. Now it appears to be becoming a lot more mainstream. What are your thoughts on how FMD has been appreciated over here in the UK and in the States?
Valter: So certainly it's appreciated. I think it's still a small group. I hope that whether it's everyday diet or the FMD, the periodic FMD, fasting mimicking diet, I hope that we can make it a lot larger and more in the toolkit of physicians, right? So we're not there yet. I think in general, we're still far, but I think now the clinical trials are coming out and the basic research has been going on for a long time, but now the clinical trials are really coming out every month or so and you see that they keep on working and I think that's what's needed to change the mentality of the public health.
Dr Rupy: Absolutely. And Elizabeth, you've got some personal experience of using the fasting mimicking diet. First of all, why don't we talk about what the FMD is and then your personal experience of it?
Elizabeth: Yeah, and may I just say that I'm a cancer doctor by training. So like some of my clients were starting to say, should I be fasting during chemotherapy? Even again, five years ago, I was saying crazy, what an idea. So just to say again that I think that's going to be a really interesting point to pick up. But I also, you probably don't know that I've been doing the five day fasting mimicking diet because in my genes, I've got obesity, type two diabetes. Mother said to me, you're just going to get diabetes, there's no hope for you. So I, you know, watched your talk at the European Congress for integrative medicine and thought, I'm doing it. So we could talk about that.
Valter: Oh, great.
Dr Rupy: Let's talk about it. What's your experience with it?
Elizabeth: Well, I think there are really some important things just at a very personal level, which is that first of all is the cost. So my husband was saying stupid idea, you know, paying this money. But what happens when your five day box arrives is that that's everything you're going to eat. You start to forget about food or shopping. But the other thing for me is that I took it as a spiritual practice, a meditative practice. I came into the zone for the five days and I was amazed like the first night powerful dreaming, directing me. So I thought, okay, this isn't just about not eating. But boy, oh boy, did it help me a few things. One, one is that I ate three times a day every time I'm hungry. So that's it's designed so that when you're hungry, you do eat something. Okay, it's not very much, but you eat something. The other thing is that I wasn't getting my normal headaches, I wasn't getting weak. And day four, I was running on air. That that kind of metabolic flexibility that I know I haven't had genetically, that by day four, I started to really feel it. Just to say the second time I did it, I didn't carve out those five days in the way that I really needed to. And I struggled a bit. I was kind of dodging it a bit. But I'm going to do my third one and that actually should be enough for me just to, you know, get where I want to get in terms of weight and abdominal weight and, you know, proving to the world I don't need to get type two diabetes. I have a really great diet by the way. So it's it's not like I wasn't doing lots of good things, but for me, the five day has really had a, you know, I've lost half a stone now, couldn't because menopause, insulin resistance, maybe whatever. So I really feel that it's helping me as an individual, but I really want to start helping my patient clients as well.
Valter: And this I think is a good example of what changed since last time we spoke. We just had a trial with 100 patient with relatively healthy people. And that was followed by three clinical trials randomized. One just was just published by a group in Heidelberg looking at the diabetes patients and diabetic nephropathy. And particularly with the HA1C, with the with the insulin resistance worked extremely well. Also the medication, lots of patients were able to reduce medication. And they did it was interesting the way this this published trial was done, it was either the fasting mimicking diet for five days a month for six months, or it was the Mediterranean diet for five days a month for six months, right? And the Mediterranean diet did absolutely nothing. And the FMD, you can see this really remarkable changes. And I have to say I had not very little to do other than telling them how to do the trial. So I like these trials, although I'm I'm disappointed I'm not the last author, but I like them because they're truly independent and this is not a group that was trying to please me or anybody else. And so and there's two more, you know, Leiden finished their 100 patient trial on diabetes. And I can say that certainly very, very positive. And we finished one in Tennessee on hypertension, lots of people with high glucose levels. And then, yeah, there's a few more around. So we're starting to get to now maybe three, 400 patient type trial, multiple sites, very, very similar results. And so it looks like about the the unlocking of the insulin resistance lock, let's say, right? So I say the winter mode and the summer mode. The summer, you're you're locked into the fat accumulation mode because a lot of food historically, and in the winter, you start burning it. And I think everybody's stuck in this summer mode, right? This this accumulate as much fat as possible. But then we also seen benefits that are independent of the weight loss. So we're starting to see both the weight loss dependent effects and the weight loss independent effects doing some statistical analysis. So it's very interesting and we're we're very, very excited, you know, for the first year ever to to to see this clinical overwhelming data.
Dr Rupy: Yeah, that's sort of the pinnacle of where you want to get to where you have multiple centers doing replicable studies that you've done in your centers, independent of your meddling or your, you know, your direction. So that's that's really encouraging to see. I think the mechanisms that you just described there, I think are very telling. Also, I know from your practice as a as an oncology doctor and oncology practice, this FMD and its utility in in treatment is very interesting to you as well. I wonder if we could talk a bit about about that.
Elizabeth: Yeah, just that, you know, you don't want to stress people, you don't want them to lose weight, you know, and yet this kind of resting phase that can be so important for people while the chemo's doing its job for the cancer cells. So I really just want to ask Valter, you know, just to help me really understand how one cares for those elements because I know that that will be a worry for a lot of mainstream oncologists.
Valter: What do you what do you think is the worry?
Elizabeth: So the worry would be that someone undergoing chemotherapy over a long course who's quite weakened and a bit vulnerable, then for them to fast, you know, like how do we how do we make that work?
Valter: So same as for diabetes and prediabetes. Now we're getting to the 5, 600 patient tested in formal clinical trials with the FMD. And we have excluded very few people, surprisingly, right? And and now lots of the trials are including phase angle measurements. So muscle function, muscle loss, either the DEXA or other impedancemetry. And and as we've seen for non-cancer patient, there's very little lean body mass loss. And I'll show it today. And so now there's the third or fourth clinical trial, very consistent results. Now, in the trial in Genoa with hormone therapy, you know, before we start, the and we we gave the doctors and the patients a video to do a very light muscle exercise for 20 minutes, I think it was four times a week. And they surprisingly, they the women on average gained muscle mass and gained lean body weight function. And so, yeah, so I think that maybe we exaggerated in the case, or they exaggerated because they're they're feeding between cycles was probably too much. And I was fighting very hard because I said, you know, if you're a cancer, if you're an oncologist and a cancer patient, your biggest fight is the cancer, right? And the second biggest fight is then the weight and the muscle, but you got to focus on the cancer. And so in this case, there is a silos and in one silos, you have the doctors at the hospital in Genoa that were worrying about the weight and only the weight. And the other silos was the oncologist who was afraid of telling the of listening to us and telling the the weight doctor, the diet doctor, no, no, no, let's keep them, you know, that's okay. We can push them, not over the edge, but certainly to, you know, keep the normal lean body mass. But I lost that fight and I think it probably was not good at all for the for the cancer, right? It was okay for the patient, but not for the cancer in these patients. And so that's a discussion to have very quickly because this is, you know, now Vernieri, University of Milan, the cancer center there they're about to publish a new study and out of 100 patients, they're starting to see what they call exceptional response in about 5%. Regardless of the cancer, pancreatic cancer, colorectal cancer, where they're starting to see cancer-free long-term survival in the type of patients that you would say, there's no way that this patient is going to live a long life. So, yeah, so I think it's it's important to to generate sort of like a working group that says, okay, we don't want to put anybody at risk, but could it be that if we combine the standard of care with the fasting mimicking diet, we can get this exceptional survival maybe in 20, 30% of the patients. And so, yeah.
Dr Rupy: Just to anchor the listener, because it might be unclear as to why we're so worried about weight loss in cancer patients. Traditionally, it's associated with a worse outcome when it comes to chemotherapy. If you see weight dropping off, it's usually not a good sign. And so when you see weight dropping off, even though it might be lean body mass, you can understand why it sends alarm bells to oncology doctors. Have I got that?
Elizabeth: Yeah, definitely. That is why it would send alarm bells and but it feels like you're getting that conversation across. And I guess listening, I also wonder about those exceptional patients, whether they're also doing other things, because we know that the empowered person is actually trying to break through to be doing other things. That's why they've often come to me and said, you know, what about fasting? But they're already doing a range of other things like mistletoe, diet, exercise. Are you looking at that element as well of how to put things together on the integrative approaches side?
Valter: Yes, absolutely. Mostly the in between diet and the and the exercise in terms of of muscle training just to make sure they don't lose weight. And we're we're not trying to do too many things because this is what we understand. We understand how to fight cancer with this fasting mimicking periods and we understand how to fight it long term and we that knowledge was gained for from cancer prevention, right? So we're combining all the, you know, 30 years of work in cancer prevention, anti-aging, cancer prevention, and then we're combining now with the cancer treatment part of the nutrition. And so, and so that I think that, you know, what I call the longevity diet, this, you know, mostly plant-based, low sugar, relatively low protein, diet that is high in in legumes and some fish, etc, etc. So that I think I'm pushing for it become, you know, central in in cancer treatment, while, of course, the physician makes sure that the weight function, I mean, the muscle function and the muscle loss is not there, right? So I think that that's what we are achieving clearly in many trials now, maybe 10 trials. And I think now we just have to bring it to to everyone. And and I think it takes a team, right? I think it takes maybe like a molecular biologist, a dietitian and a physician working together. Sometimes it takes an integrative, we've done it with integrative doctors, integrative medicine doctors. Those are the usually the ones that can sort of maybe do it all, you know, oncologist plus integrative doctor, or maybe an oncologist plus a molecular biologist and a dietitian. Those two teams seem to work, yeah.
Dr Rupy: Yeah, yeah. And you've spoken about this before about how fasting as a term is very vague. It can mean a number of different things. We're specifically talking about FMD here, fasting mimicking diet, which is a five-day protocol. Are there other methods of fasting that perhaps are more appropriate for different people that you believe could be as effective? And are there any human trials that you're aware of looking at those modes of fasting as well?
Valter: Yes. So I just published a book in Italy on cancer and fasting. And hopefully it will come to the to the well, it's going to come to US next year and hopefully to the UK. And in that, we talk about, for example, this large study where they they showed the correlation between 13 hours of fasting or longer daily and progression of breast cancer in breast cancer patients, right? So that's definitely a recommendation. Yeah, go for about 13, 14. Normally I say 12 for everybody else, but I think for the cancer patient, it seems to be the side effects of going longer than 12 are probably overcome by the potential benefits. Benefits that are now shown to be true, they're associations, of course, right? So we don't know, but you know, the women that fast more than 13 hours do better. So yeah, so that's that's for sure one of the the ones. And now, I think that's probably it, right? I don't think you start introducing too many things and then and then you can start seeing side effects. Like say every day fasting, now 5:2. I mean, there's all kinds of things you could do, but we as you mentioned, fasting means nothing. Like eating, fasting was what does that mean? You know, if you want to move this into the medical field, even though I get attacked sometimes, oh, but because he's trying to sell, I'm not trying to sell anything because I give everything to charity. So this is definitely not it. But I think I realized the standardization, how important is to standardize it for the physicians all over the world, whether it's Japan or South America or the UK. So it's got to be standardized, got to be tested clinically. And then maybe then the the the physicians will start will start applying it, you know.
Elizabeth: I would love to ask Valter this because when I put on to social media that I was doing a five-day fast, I got people saying, oh, you know, you should be doing whole food, shouldn't be doing this fasting. What what what are your thoughts about people who are doing kind of replications of the five-day fast but using whole food?
Valter: Yeah, it would be like saying, you know, rapamycin comes from the dirt of some island, Eastern island or something like that. You know, what if what if the pharmacist and the physician said, you know what, you could do it yourself, you know? You got, you just got to transplant. That's what rapamycin is used for. You just got to transplant. You just pick up some dirt and then, you know, you grind it up and yeah, of course, the FDA, we went to the FDA now for hormone therapy and cancer treatment, right? It was a long, excruciating set of discussions. And then they said, okay, you got this box? No, right? Let's take this box and let's make it into 14 ingredients. And you tell us exactly what's in it, and you tell us where you're going to pick the food to make that and how you make it. And maybe, maybe in two or three years, we'll let you do that, right? So you see now the established medical system, how far it is from, oh, I'm going to go home and and it was one of the guy, the former director of the FDA, you know, we had this discussion and I said, you know, I think we know why it's working for cancer, etc. And he told me, you don't know. You think you know. But what if it was one of the ingredients, you know, that you're adding that for some reason is triggering the microbiota, which is signaling to the immune system, which is causing immunotherapy, an immunotherapeutic like effect. And it has nothing to do with what you think is working, right? I mean, of course, it's very unlikely, but what if? That's what he said, right? You know, that's make a very good case, right? So, so, so yeah, so that's that's why it needs to be standardized. And I don't mean we need to spend a billion dollars and, you know, take 10 years. I think it should go very fast, but it needs to be very standardized. And I think this lifestyle program, now the FDA allows that, says, okay, if it's not a drug, I'll allow you, you standardize it, you show me two, three, four clinical trials, you show me consistent, like you were saying, multiple side doing it, make it, you know, convince me that that it's true with statistics, and then I'm not coming after you. And you can use it together with muscle training, together with a good diet in between, and use it in combination with standard of care, right? I think that's this is the way to move forward, much faster than getting FDA approval, but this could change things around from what we've seen now in many trials.
Dr Rupy: What I what I also think is exciting is that, you know, working in cancer over many years, it was always like, yeah, all of this is important in prevention, but it's not important in treatment, and you should just go away and have double cream and digestive biscuits. And I think what's really exciting with the work that Valter's doing is, you know, making it part of an integrative approach, a treatment during cancer treatments. And for me, the really interesting thing is survival, because, you know, maybe not just this element, but other elements that people can take on, could we really start to turn things around, not just for cancer, but for other long-term conditions as well.
Valter: Yeah, absolutely. And I think the application of this to other conditions is really telling of how you're really getting to the root cause. We talked a little bit about the mechanisms behind why it might be working for things like weight loss, even for for cancer. What are the other mechanisms that are going on that you believe or you hypothesize are happening when someone goes on the fasting mimicking diet? And just another point is that I definitely appreciate that about the FDA approval because I think when you're measuring exactly what goes into every element of the five days, you know what the micronutrient content is, what the phytonutrient content is, the macros, etc. So that's very important if you're going to prove this model out for various specialties in medicine as well.
Dr Rupy: So mechanisms, of course, we and now the good news is it's expanded to many laboratories all over the world, like animal studies and all that. But for example, the one we published last year for for hormone therapy in breast cancer, we showed, I mean, and in the early days when I used to talk to oncologists, it used to be like, oh, yeah, yeah, yeah, the fasting mimicking diet, like, you know, I heard there's a story about carrots, people that eat more carrots, they benefit more, right? So they were not taking us very seriously. It was almost like, yeah, okay, like you were saying, but what could this possibly do? And if you look at that paper, which by the way is published in Nature, you see how the fasting mimicking diet is knocking down leptin, insulin, and IGF-1, all three, plus many other things. But these three, any of these three could make the cancer start growing again. So it's palbociclib, fulvestrant, two hormone therapy, CDK4/6 inhibitor, two drugs that are used standard of care, plus three different markers that are now or factors that are now downregulated by the fasting. So now imagine that you had to have come up with five drugs, which by the way, you don't know what they are. So it could be these three drugs for one patient, it could be that all of a sudden IGF-1 is no longer important for that patient and glucose becomes important, right? Because now we saw that for stem cells, for cancer stem cells, glucose was important. For differentiated cancer cells, glucose was irrelevant, right? So now you have to lower, it was four actually. So glucose, leptin, IGF-1, and and insulin, right? So that's what the the field is not appreciating, this wild card effect, right? Revolutionize the system, create a differential property, differential effects. Normal cells, they know exactly what to do, right? They don't care if IGF-1, leptin, glucose is low. They've seen it starting in bacteria 3 billion years ago. The cancer cells, they just don't care what the environment it is, they're just going to keep on going. By definition, by the way, it's not my definition, it's the hallmarks of cancer. So, yeah, so that rebellion sets them up for failure. But what do we do in the clinic? As you said, eat some donuts, right? Because you're not feeling so good, so maybe eat some donuts, feel better. Well, guess what? That donuts has got carbohydrate, and this carbohydrate are going to help, in this case, those cancer stem cells, and that was enough to get you in the long run. We could drive the cancer down, regression, and then the cancer stem cells slowly because of the glucose took over and the whole thing happened again, right? Even in mice. So, so yeah, it it's a very complicated, but I think we're the the field and not just because of us, many, many labs is getting sophisticated enough to where we're like now can can sort of smell that we're almost there, right? We're we're almost starting to understand so much about the cancer that we can we can trick it into doing exactly the things that will cause every single cancer cell in the body to die, right? I always give the analogy of the of the desert, right? You take a billion people, you put them in the desert. Well, if you give them water, if you give them shade, and if they sit down, you know, after a couple of weeks, you're going to have a billion people alive. If you take the same billion people, you make them run, no shade, and no water, you know, two weeks later, probably zero survival, right? So, yeah, so this is what we're we're looking at, this differential properties of of of living systems.
Dr Rupy: Yeah, absolutely. I think it goes hand in hand with metabolic medicine as well. I think a lot more people are talking about it as is evidenced by this conference. It seems to be on the tip of everyone's tongue. In terms of, we've talked about cancer, we've talked about weight. What other areas do you think it could be used that we're not really talking about today?
Valter: Yeah, I think for autoimmunity seems very, very promising. We have one trial running in Genoa for multiple sclerosis. We have two at Stanford for IBD, both Crohn's and colitis. And, you know, a number of other hospitals that that are now looking into, you know, different autoimmunities. So, yeah, so I think that it's got a lot of potential. We published the mouse data, looks very promising, but the human, we published one trial at Charité, a collaboration with Charité neurologists, and it looked very promising, but of course, it was a multiple sclerosis, it didn't have MRIs. And so the criticism of course is it's too early, let's see what happens. It's like cancer 10 years ago, right? So we're in the early days of autoimmunities. But I think what is emerging, because somebody listening and say, oh, what is it a miracle now it works for everything. I think it's about maybe fasting was always there to fix problems, right? I say you cut yourself and within a couple of weeks, that wound is perfectly repaired. What if you go to sleep and at night, there's a lot of things being repaired, right? What if fasting represented that periodic moment where everything goes to work to repair. So autoimmune cells probably don't belong there, let's eliminate them. Pre-cancer cells don't belong there, let's eliminate them. Insulin resistance, okay, that maybe it's no longer the moment to be insulin resistant because the winter is coming, let's reverse that, right? So that's a possibility. I know it's a it's a it's a big claim, but certainly when you see it working with all these different conditions, now we're working on Alzheimer, right? So we have a clinical trial in Genoa, Perugia, it's into its it's about a one year into it. And we're about to publish on the mouse work. So it's just it would be the coincidence that it's working on all these things is unlikely. And so, yeah, possibly some some fundamental role, evolved role for fasting itself to to fix things.
Dr Rupy: Yeah, absolutely. I think the drawbacks of fasting in general are and what should we be looking out for to make sure that we're not tricking ourselves into believing something exists or some mechanism is there when it doesn't?
Valter: I don't like this idea that because fasting and fasting mimicking diets are good for you, you should do it all the time, right? I think it's not, it's not a good way to go. And and I'm I'm worried about that. I think it's about you do it when you need to do it. And so it could be, it could be that eventually it turns out to be great if you do it, say 12 times a year. But I think right now, I'm I'm more comfortable with let's say, you know, two, three times a year for people that are healthy. And you know, in the clinical trials, yes, we see six cycles a year or so working. And in the one in Heidelberg that just published, they did six cycles and then they waited three months. It was a washout period. And then at nine months, it was still significant. The A1C, the insulin resistance drop was still significant. So I think that that, yeah, so then let's say two to three going all the way to probably six or so for the diabetic. That seems like a good, of course, the diabetic has got a real problem and and you can't say, well, maybe in 20 years, if I do six cycles, I'll have some side effect because, you know, you have to worry about the diabetes. And the same is true for for cancer, right? So, so you got a bigger problem to worry about than whatever hypothetical issue may may happen later. Yeah. So I think that again, for for the fasting mimicking diet and the fasting field in general to to go forward, we have to be a lot more rational and we have to be a lot more careful. And I think this is got to shut this time to to become part of standard of care.
Dr Rupy: Yeah, yeah. I think it's it's really important and that's a great point about being cautious with overusing a tool. At the end of the day, we have a selection of different tools. And on that on that topic, let's say we have someone who is in general good health and wants to optimize their health. How do they objectively decide whether two rounds of FMD in a 12-month period is useful or four or six? Are there specific markers that people should be looking out for to determine what is the sort of Goldilocks amount of fasting?
Valter: Yeah, I think that probably good to look at all the main markers, you know, so where is your A1C? What about your cholesterol? What about your blood pressure? So, you know, very, very few people after let's say age 30 are perfect, let's say, right? Very, very few, maybe 5% or so. So, so, you know, your blood pressure could be 132. And maybe it was 125, then it went 128, 130. So you're moving in the wrong direction. And then, you know, the cholesterol was 175 and now it's 207. Yeah, so that that person might need to do it three times a year, every four months. And and that may may help or should help, you know, based on the clinical trial should help. We've never done it like that and we're doing it now. We have about to start a 500 patient trial in Southern Italy where we're going to randomize three groups, control FMD, FMD plus longevity diet, right? And so I think I hope that's going to be much more conclusive. And and I for the first time, we're going to do it every three months. So in the trials that we've done so far is every month for three months. And then we we look at three months later without doing it and it's it's still impressive, I think even three months later, the effects are still there, but you see them they're starting to move in same as in the Heidelberg trial, right? Three months past the six cycles in the diabetic patients, you see that them going back to the same lowering of insulin resistance that was there at after three cycles, right? So, yeah, so it's slowly going back. So it tells you that between three and six months, lots of the effects go away if you if you return to a your normal whatever you you did before, right? So of course, yeah, if you change your diet, it could be that and that's maybe the answer, right? So if you start doing all the things right and you eat the everyday longevity diet and you exercise, etc, etc, you know, maybe a couple of times a year would be enough. But for the great majority of people, and and then also depends genetically, who are you? Do you have high cholesterol to begin with? And, you know, do you have cognitive issues? Do you have inflammatory issues? You know, is your CRP high, right? So I think you have to look at the whole thing and and decide where you want to be and see how the FMD helps you get there. And I would say the great majority of people we see them we see them being helped by by the by the FMD.
Dr Rupy: Yeah, yeah, absolutely. I think I guess the danger is to ensure that people don't slip back towards the baseline as they take away the tool. It's sort of like on a calorie restricted diet, someone will definitely lose weight and they'll plateau and their numbers will improve, blood pressure might improve, depending on the cholesterol, that might improve, depending on the diet that they're on. But then as soon as they come off that diet, it comes back up and you change your weight set point and then you see on the graph, it's just trending upwards. So I guess it would be very interesting to see if FMD as a very nice applicable short-term intervention that can be routinely applied could maintain a baseline that's actually steady across.
Valter: Yeah, that's what we see, right? That's what we see. And and I always I'm always entertained by these studies on long-term, you know, very severe restrictions, like 800 calories for six months. And and you know, and those are I'm surprised that some of the big journals are publishing this because we all know what happens, you know, after that. And on top of that, they they're not aware of the studies showing a metabolic slowdown, right? And which by the way was published in the New England Journal of Medicine many years ago and you just we keep on forgetting all studies, right? and keep getting back into there. So, so yeah, if you do restriction for a long time, your metabolism seems to slow down. And now even adjusted for your body weight. So your body drops over 10% and your metabolism may slow down 15%. So now you're in trouble because what is that telling you? You got to regain your weight, right? It's it's giving you the signal, go back to where you were because I was happy where you were. And that's hard to fight evolution like that, right? So yeah, so the the FMD, we don't see that. That doesn't mean it's easy, but because it allows you after five days and probably for about four months to go back to whatever it is that you were doing. And I I really think it's a it's a something that could but whatever a fourth to a third of the the world is in some pre-diabetic to diabetic state. Yeah, so I think that's that's a group that should use it like that, like you just defined. Okay, I'm I'm going back. I used to be fasting glucose 90, A1C was 5.4, now I'm 5.6. And I think in the UK is a different unit. Yeah. But but, yeah, let me let me do one more FMD, maybe introduce a little bit more of the components of the longevity diet. And and that's how without drastic and that's, you know, we have two foundation clinics, one in Milan and one in Los Angeles. And that's a recommendation we give to all the nutritionists, don't make anybody revolutionize their diet. It's never going to happen. So just go with with small changes that I think can have a big effect. And I think 15 days a year, it's a small enough change that the great majority of people, especially those that are pre-diabetic, they're looking at life, oh, you know, maybe in six months, I'm going to be on metformin and then and then when does it end? And today, I'm going to end my talk with a physician in Italy, 67-year-old physician that was diabetic and hypertensive, went to his friend and his friend told him, I'm sorry, I'm going to load you up with drugs. And he did, right? He's on a professor, university professor, endocrinologist. And so he does that and gets worse and worse and worse. And then we move in and, you know, in two years, it's back to like no drugs, no problem, no. Yeah. So it used to be an anecdote. Now it's clinical trials, right? So, so yeah, so I think that we are excited about this, you know, seeing the physicians, you know, doing it and seeing the physicians saying this is a very reasonable and and doable way to to get there.
Dr Rupy: Yeah, I completely agree and I can definitely see the appeal to both physicians and patients, particularly when there's going to be a lot more robust clinical trials out there on on humans. Just to draw this conversation to a close, the longevity diet, love the longevity diet. You know me, I'm I'm into my nutrition and healthy eating. I think it has to be a flavorful, delicious diet that someone has as their baseline. You you have some views on low protein as well. And I wanted to ask a bit about how low is low and if that low protein applies to everybody across the spectrum and whether there are instances where there might need to be more protein, let's say women during the during the perimenopause and menopause or maybe some other aspects of of where a low protein is is not recommended.
Valter: Yeah, for for lots of people, right? So for example, I wrote a book for children and diet and we recommend a higher protein than than the 0.8 grams per kilogram that we recommend to all the adults. And then we published a we published a meta-analysis on IGF-1, which is dependent on proteins, and we published a paper on protein levels showing that over 65 having too low of a protein diet was detrimental, was associated with a lot of problems. So it looks like let's say in the 20, 25 to 65 biological age, by the way, right? So doctors pretty soon, whether they realize it or not, it's about the chronological age era is about to end and the biological age era is about to begin. So, so then the doctor is going to have to say, well, you really are 64 biologically, even though, you know, chronologically you may be 73, right? And then, yeah, so there is a point where people start losing weight around 65 on average. And that's a point probably where too low of a protein could be a problem. And so, yeah, so then imagine somebody who's 100 pounds, we're looking at maybe, um, you know, 37, 40 grams of protein minimum. Now, it gets tricky because if most of your proteins are from legumes, now you're going to have very low levels of a few amino acids and that's not so good for you, right? So this is why we move to, you know, interesting enough, the old diet of my region in Italy, Liguria, which is pescatarian, right? So lots of legumes, lots of vegetable, but enough fish. And and the other place that has that is where Ancel Keys did his studies in near Naples, right? Yeah. So fish because they were poor and that's all they had. And lots of legumes and lots of vegetable. And it turns out that Genoa is now one of the highest percentages of over 65 in the world. And, you know, and Ancel Keys made the region near Naples famous for for the Mediterranean diet, you know. But I think now it's like a pescatarian diet of a sort very careful dosage of of fish and the right type of fish seems to be the ideal diet. And I just published on that. And so I encourage everybody, it's a it's a paper in Cell that just came out a couple of months ago and it's, you know, people can download it for free. So I encourage everybody to to to look at that.
Dr Rupy: I will link to that in the show notes for sure. And what's your favorite fish?
Valter: Salmon. Not necessarily my favorite fish. My favorite is tuna, but it's packed with mercury. So, so there you go, you know, I eat it maybe once every two months or so, but I eat salmon maybe a couple of times a week.
Dr Rupy: Yeah, yeah. Oh, that's good to know. I have a lot of oily fish in my diet as well. And how many, how often do you do FMD in in a year?
Valter: Probably a couple of times a year, yeah.
Dr Rupy: Okay. Yeah, yeah, yeah. I'm going to try it and I'm going to, because I've only done various, I've done various methods of fasting, but not a full five day FMD. So I'm going to, I'm going to do it and I'll report back to you and I'll let you know what my numbers are as well.
Valter: Yeah.
Dr Rupy: I look forward to the the new research. We'll probably have to get you back on the podcast when it's out and I wish you well with your your lectures today and the next pods.
Valter: Thank you.
Dr Rupy: Yeah, appreciate it.