Dr Rupy: It's a slow burning process, that's the problem. And it's insidious and it creeps up on you. We've got to recognise we've come out of COVID, cost of living, all of those things that aren't, they're life, we're humans. They're life. And there's a whole bunch of people that are working to make ends meet and and challenging circumstances, and they feel fine. Do you honestly think they're going to worry about this until they are? Then they're going to see a doctor. And that's not what really health system should be about. It should be about preserving health. But that basically means you've got to speak the language of those people, to bring those people in, to engage with those people in a better way than we've done.
Dr Rupy: Welcome to the Doctor's Kitchen podcast. The show about food, lifestyle, medicine and how to improve your health today. I'm Dr Rupy, your host. I'm a medical doctor, I study nutrition and I'm a firm believer in the power of food and lifestyle as medicine. Join me and my expert guests where we discuss the multiple determinants of what allows you to lead your best life.
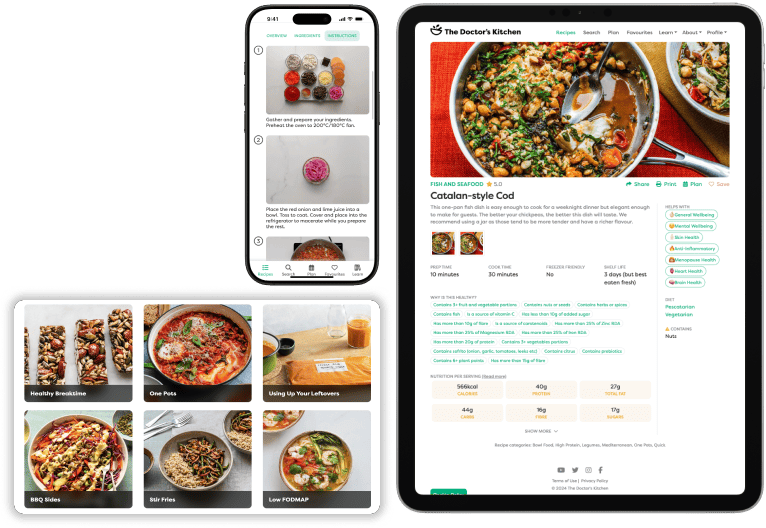
Dr Rupy: Something that I've become a lot more knowledgeable about after my training as a general practitioner is cholesterol. It's probably the most important measurement every primary care doctor should know about. However, it's the least well understood. Now, obviously cholesterol goes hand in hand with other measures of metabolic health like weight, insulin resistance and blood pressure, but I think we do a disservice to our patients if we don't know the intricacies of what is a critical measure of our heart health. And on today's episode, we're going to be doing a deep dive into all things cholesterol and cardiovascular disease with Professor Kausik Ray, who's Professor of Public Health and Honorary Cardiologist at Imperial College London and President of the European Atherosclerosis Society and perhaps the most knowledgeable person that I could talk to on this subject who has both research and clinical expertise in this area. Now, there will be a few things I'm going to reiterate right at the start of this podcast to prime you, the listener and viewer, to keep you on track, because we do get quite into the woods in this episode. So I just want to make sure that this is as understandable and actionable as possible. At the start of our chat, we define exactly what we're referring to when we say cardiovascular disease and atherosclerosis, what that entails and why it's important being the leading cause of death globally. We then reaffirm the importance of cholesterol in the body. Without cholesterol, there is no life. Cholesterol is the precursor to our hormones, it forms the structural components of our cells, and most of our cells are able to create the cholesterol we require, hence why there is no nutritional need to consume cholesterol. There is no such thing as good and bad cholesterol, just cholesterol. We measure cholesterol indirectly by counting the number of cholesterol taxis in the body because cholesterol is not able to travel in the blood. And the common ones that we talk about are HDL and LDL. These are high density lipoproteins and low density lipoproteins, although there are other cholesterol carriers that we also refer to. At the end of this episode, hopefully, you'll learn more about why the trifecta of high cholesterol in the blood, high levels of inflammation and damage to the arteries leads to disease, what blood measurements we should all have to calculate our risk, which include apolipoprotein B containing lipoproteins, non-HDL, and something called LP little a, as well as the strategies to reduce risk with drugs and lifestyle. Now the aim of strategies to reduce heart disease is to reduce the presence of particles that are able to penetrate arterial walls where the cholesterol cargo can be damaged, inflamed, and that leads to the process of scarring of the artery walls, something that we refer to as atherosclerosis. We also make note of something called LP little a that I've just mentioned. This is a particularly atherogenic particle, it's particularly aggressive, and elevated levels of LP little a are primarily determined by genetics. This is an independent, significant risk factor for heart disease and unfortunately, it's largely unchanged with diet and lifestyle, and the current treatment revolves around optimising other risk factors. We talk about exactly what LP little a is at the start of the podcast as well. We also refer to medications and pharmaceuticals to control cholesterol levels and why even when people have low levels of LDL cholesterol, people still suffer heart attacks, and that's because of a concept known as residual risk that again we talk about. I've done other episodes on the Doctor's Kitchen podcast about specific foods and dietary patterns to reduce cholesterol, but I think this is a necessary episode to give you the backdrop as to why this is important for everyone to know their numbers. Everyone should know their numbers. And currently, I don't think the standard lipid panel does enough to cater for everyone's individual risk profiles. And I'm a firm believer, even more so now, that we should be looking at other markers including LP little a, which is something that you just do once, and non-HDL or apolipoprotein B levels. These are much more tightly linked to a true risk of cardiovascular disease. If you want to know about what you should be eating for heart health, improving blood pressure and lowering cholesterol, one of the reasons why I made the Doctor's Kitchen app is to make it easy for people to understand how to use food in a medicinal context, which is why when you go into the Doctor's Kitchen app, we do a long quiz, and on that quiz, we ask you about your health goals. One of which is heart health, including lowering blood pressure and lowering cholesterol as well, because it is a real confusing minefield of information out there. And so when you click on the heart health category, you can be sure that we've done the hard work for you. We've gone through the studies, we've looked at the dietary patterns and the ingredients that align with that particular health goal, whether it is lowering cholesterol, or improving menopause symptoms, or reducing the risk of dementia. It all is done by us in the background, so you can just cook delicious, flavourful food that give you variety and balance every single week. I'm also pleased to be bringing you this podcast in partnership with Exhale Coffee. They are the official sponsors of the Doctor's Kitchen. I'm also chief science officer, which means that I'm going to be across all the different products in their categories that will be coming out in the future. I absolutely align with the mission of Exhale. I've been an advisor now for almost four years to Al and Kirsty, and I just think small businesses have the power to ignite the change that we need to see in food, both being nutritionally balanced, flavourful and at a price point that people can afford with true transparency across the production process. And Exhale coffee is not just ridiculously healthy, it's ridiculously tasty as well. And I'm a proper coffee snob. So if you want to try coffee for the first time, you'll get 50% off a subscription, just click the link that says try Exhale coffee in the caption of your podcast. I'm sure you won't be disappointed. For now, please do enjoy my conversation with Professor. And if you want me to go deeper into any of these subject matters to do with cardiovascular health or cholesterol or a more food specific one, then shoot us a message at the app on Doctor's Kitchen or just on Doctor's Kitchen website, we'll be collecting feedback from all of our episodes. And you can also shoot us a comment on YouTube as well if that's where you prefer to leave your comments.
Dr Rupy: Professor, thanks so much for coming in. We're really excited to dive in deep into all things cholesterol and heart disease. I really want to give people an insight into what it's like to see you in a both a clinical context and an academic context. So I thought we could start off this conversation by just going through a few definitions because from my understanding, there is a lot of confusion for for folks who hear these terms like heart disease, atherosclerosis, CVD. Why don't we talk about some definitions that people should understand before we dive into this conversation. So what do we mean by atherosclerosis?
Professor Kausik Ray: So atherosclerosis is referring to the process where if you think about the blood vessels as pipes, is the build up of fat over time in the walls of the blood vessels and the body doesn't like that. So it responds by trying to accommodate that, wall that off, building scar tissue. And that combination of scar tissue and fat in the wall is what we call atherosclerosis. And the reason that it is actually so important is, well there's eight billion people in the planet. And so if you think about over a period of time, all of this is kind of going on. And when that lining over that atherosclerotic plaque, that that area becomes unstable, then when that fat comes into contact with blood, that's when you get a clot forming. So if it's in the heart, that would be a heart attack.
Dr Rupy: And where else do we get atherosclerosis?
Professor Kausik Ray: So you can get atherosclerosis throughout the body. Typically, we tend to see it in the the blood vessels that supply the heart. We'll see it in the main pipe, the aorta that goes down the body from leaves the heart and that essentially branches off and supplies blood to your organs and goes up to your head, down your legs. Typically when we think about strokes, for example, we think about the two blood vessels, the carotid arteries getting furred or narrowed. And then we think about something called peripheral arterial disease where the blood vessels in the legs get narrowed. And so these are people, for example, that complain of pains in their legs and their calves when they walk.
Dr Rupy: And when people hear cardiovascular disease, heart disease, are these interchangeable terms? Are they distinct in certain ways? How do we think through that?
Professor Kausik Ray: So so if you like, some of these are subsets of the other. So heart disease is a subset of cardiovascular disease. So cardiovascular is the heart and the blood vessels. So if you're thinking about cardiovascular disease, an easy way of maybe thinking about this is when you think about the heart in particular, there are things that can happen that involve the pipes, so atherosclerosis, heart attacks, to the blood vessels of your your brain, strokes. You can think about electricity, so the the wiring, these are things like irregular heartbeats. So atrial fibrillation, an irregular heart rhythm increases your risk of stroke. You can think about the heart valves, for example, so either leakage or narrowing. And then you can think about the heart muscle. So all of those would be cardiovascular, but they have different causes, they happen at different ages, different risk factors, different genetic backgrounds.
Dr Rupy: And dyslipidaemia?
Professor Kausik Ray: Yeah, we've not done ourselves huge favours in medicine, have we? So typically when we're talking about dyslipidaemia, it's a broad spectrum because there your and we can talk about the the what you measure in the blood. Typically when we think about dyslipidaemia, we're talking about elevations of cholesterol. It can include also elevations of triglycerides, and it can also include lower levels of something called HDL cholesterol, which lay people would would term good cholesterol, but there's no such thing as good cholesterol.
Dr Rupy: Let's let's double click on that point as we've just talked about good and bad cholesterol because I hear these terms a lot even with, you know, well intentioned general practitioners and other folks. Why is cholesterol, cholesterol, cholesterol rather than good, why than good cholesterol and bad cholesterol?
Professor Kausik Ray: So if you think about the what circulates in blood, fat doesn't mix with water. So cholesterol is carried at a microscopic level if you will, in something that we call lipoproteins. So they're like spheres, they're like, you know, when you when you look at these sci-fi sort of movies and you see the atomic scale, it's a big sphere, it's a planet if you will. At its core, you've got cholesterol or triglycerides. And triglycerides are an energy source. Cholesterol esters as they're called, are involved in for example, hormone synthesis, they might be involved in making the the walls of your cells, what we call cell membranes. And the best way of thinking about this is there are three main taxis that carry cholesterol towards the artery wall, causing damage. And there are three particles. One is the low density lipoprotein, LDL particle. One is something called lipoprotein A, and one is a particle that contains triglycerides. These are slightly larger, and they also contain cholesterol. And on the surface of all of these, there's a protein called apoB. So if you like, that's very easy to remember, B for bad, goes in the wrong direction. Then what people call good cholesterol is really referring to a constellation of particles that we we term HDL particles. They contain cholesterol and triglycerides, but their job is to try and remove cholesterol from the blood vessel wall, take it in the opposite direction. So that also carries cholesterol, but it's its role in biology is to do something that's different. So you've got three particles effectively dumping cholesterol potentially in the blood vessel wall, and one carrying it in the opposite direction. But you don't have equal numbers of each of these. And their ability for good or harm varies. Because they they so think about for example, so if we take the example of LDL cholesterol and lipoprotein A, we can talk a bit more about that. But our kind of conventional wisdom is, imagine I've got the blood vessel wall is a is a shooting range. I've got, let's say, 10 bullets. Those are my LDL particles. I've got one lipoprotein A particle, let's say, because it's a much lower concentration circulating. But that one bullet is going to splinter into 100 pieces when it hits the wall. So that's why we think even though there's less of lipoprotein A, molecule for molecule, it might do four to six times more harm.
Dr Rupy: So we'll get on to this concept of atherogenicity, but the atherogenicity, so the harm potential of an LP little a is a lot higher than LDLc, am I correct?
Professor Kausik Ray: That's the that's the current belief.
Dr Rupy: So just to clarify, cholesterol is cholesterol, there's no different types of cholesterol, just one form of cholesterol. There are different carriers of cholesterol in the body. And the term good cholesterol that's usually assigned to HDL cholesterol is again a bit of a misnomer because we don't fully understand HDL's role in it.
Professor Kausik Ray: And the other thing about that is that came about from a set of studies that were done from largely from Framingham, this little town in Massachusetts. And what was found was that essentially, if you had higher levels of good cholesterol, HDL cholesterol, your heart disease risk was lower. Then what happens is you look at the bottom, you look at the middle, you look at the highest group. There weren't many people in that study. And there were only about 300 events and you can draw a straight line. And then in 2009, we basically showed when we looked at over 300,000 people, totality of the world data, 25,000 heart attacks and strokes, actually it's not a straight line relationship. It's a hockey stick. So and it's what's called an association, it's not causal. At about 1.4, as you get higher than that, you actually don't get any less risk. So you'll see people, for example, women will have a higher HDL cholesterol levels. And when we tend to use ratios, you're underestimating risk because you think a ratio, an HDL of three is more protective than a 1.4 and it's not. And you know, there's also now some data where very high levels might actually be a marker for sicker individuals who are at higher risk of dying. So that whole concept about HDL, low is bad, that's for certain. High doesn't necessarily give you much more protection.
Dr Rupy: And so the cleanest of those we've done recently, or colleagues have done recently, giving people infusions straight after a heart attack who had low HDL levels. And so what the belief was that if you basically gave them these infusions, you've got the particles that should capture cholesterol from the blood vessel wall, and then that should help remove the fat, they've just had a heart attack. That's what the trigger was, and it would make a difference. And it didn't. We there are drugs that we 20, 30 years ago, a drug class called CTP inhibitors that were originally were developing because we thought raising HDL was was good because we'd kind of had statins for LDL lowering. And what we then realised is actually the same class of drugs also lower LDL. And actually the the benefit that was seen in the first of the trials that showed a benefit was related not to the 100% increase in HDL, but it was to the 20% reduction in LDL. That's the the benefit was entirely predictable by that change. So so basically we've got a we've got a lot of our main focus is because you've got essentially more of those bullets if you will. There's just at a population level a lot more of those. That's why largely that's been the main focus, take that off the table first.
Dr Rupy: Might seem like a bit of a silly question, but why don't we get this disease process in veins? Why is it arteries?
Professor Kausik Ray: Yeah, so there's probably, so the one of the things about all of this is firstly, the the disease process is there's no single factor that determines this. So one of the things that we need to think about is inherited genetic vulnerability. So when people think about a family history, they think father or mother had very high levels of something which then they passed on. Probably as common if not more common is essentially a whole, not a single variation, but a whole host of genes, variations in those that just make you much more vulnerable to the world around you, which explains why the vast majority of heart attacks at a population level, if you think about the number of people that have that, have disease like that, will occur in people that don't have extreme levels. There are lots of little things that have added up. It's genes, your best days, your worst days, lifestyle, and how many years you've been alive on the planet. So seeing a little bit of disease in the blood vessels at age 75 is very different from seeing the same amount in a 35 year old. Because you know, the 35 year old, if he's got that much already at 35, way more vulnerable, the outlook's not good. Yeah, if you get to 75, then you probably are resilient to that same number, all other things being equal. So to the question about veins, probably pressure, you need higher pressure systems as well. So if you think about one of the the the points that we were making earlier on about, think about the blood vessel lining as a footpath, cobblestones. To get into the wall, you've got to get through the cracks. How do you do that? Well, if you damage the arterial wall, so if you've got higher blood pressure, you're going to get more of those particles that are floating around in blood into the wall. If you have diabetes, you make the blood vessels a bit more leaky, more can get in, maybe more is retained as well. If you smoke, same thing. So effectively, your risk of heart disease, heart attacks, atherosclerosis is happening at a lower lifetime cholesterol exposure. So somebody who doesn't have all of those things, the artery wall is less damaged, more resilient. So I need a bigger lifetime exposure. But on the other hand, if you're making that leaky or damaging it, then a small amount just getting through is starting that process. So in veins, we have a very low pressure system. And the only way you really get clotting in your in veins is when you get trauma and you typically damage the the veins and the walls and you get inflammation. So usually you get a clot, it's what's happening in the wall, the thickness of the blood and also the the flow. So you have low flow, thick supply, and you've got inflammation in the wall, that's your characteristic sort of DVT.
Dr Rupy: And so as you've alluded to, what are the driving forces behind this atherosclerotic process? So taking into account genetic risk factors, yes, we'll put those in a box. Other, you've got wall damage and that can come from direct inflammation from smoking particles. So the inflammation related to that. Pressure effects, so high blood pressure creating damage to the endothelial wall. What are the other sort of factors?
Professor Kausik Ray: Yeah, so so typically, if you were to think about smoking, blood pressure, then we we need to think also about not just diabetes and basically higher levels of blood sugar levels. But if you like, even in those people who are obese, who are overweight, who are pre-diabetic. So for example, we just published last week using UK Biobank data, asking the question, is there such a thing as metabolically healthy obese? Because you know, people have talked about this. So what we looked at was arterial stiffness, and that's a marker of vascular health or damage. So you can take people who are overweight and obese who've got none of the other lipid abnormalities, no elevated blood pressure, no diabetes, and the the stiffness of the the blood vessels is not normal. Then you can take a group of people who are not obese, who've got those metabolic abnormalities, and it's the same. If you've got both, it's even worse. So so basically, there are a whole bunch of processes that we know, clearly, blood pressure, high levels of bad cholesterol, and then you've got individual particles as well, like triglycerides containing particles could be more harmful, lipoprotein A, smoking, insulin resistance and inflammation would be the main ones. There may be other things that come out. But we know that about 60% of the heart attacks that occur will be explained by about five or six of these factors. So pretty much, so the the bulk of what we have can be explained. The bit that we don't actually usually factor in very well is time. I.e. how long all of that's been going on for. And it's the return on investment principle. If you if the changes have been there for a long time, then in a more vulnerable individual, those extra decade or 20 years is going to make a real big difference.
Dr Rupy: I like this concept of return on investment because I kind of think about it in the same way of smoking pack years. So the amount of exposure you have to all of these insults. So whether you've allowed a persistent raised cholesterol from your 20s all the way to your 50s because in your 20s you're like, I don't need to worry about my cholesterol, that's later on down the line thing, versus, you know, having it treated for a longer period of time. So you're basically giving yourself a higher exposure and increasing the probability of it lodging into the arterial wall. Am I am I correct in thinking that?
Professor Kausik Ray: Yeah, absolutely. And and the thing is that also that the age side of things is not to be underestimated in terms of the benefit. So the best way to think about that was with a with a couple of analogies. So a lot of people will talk about how many people did you have to treat to prevent one event, so called number needed to treat. Well, there's a variable there and that is what was the risk? If there isn't much risk over the next three to four years, even if something's beneficial, the gains are going to be small. I mean, you know, you need to be at risk. So if you drive, a seatbelt's beneficial, period. But the chances of it saving my life are going to be more if I'm driving every single day at 70 miles an hour rather than in a cul-de-sac once a week where the maximum speed is 20 miles an hour. So that's the relative and the absolute. The relative benefit is the same in both scenarios, the absolute is different. And and I think that the the issue that we have is that people think about having to have symptoms before they've got a problem. So you need a lot of narrowing of your blood vessels, whether it's your legs or any or your heart, before you complain of chest pain. You know, supply and demand phenomenon because the body's been able to adapt and cope and accommodate up to a certain level. But that process was going on decades before it shows up. And the worrying thing is that about 50% of people, the first presentation is with a sudden death because of a heart attack or a heart attack that doesn't kill you. You go into hospital, you open up the blockage, but actually unless you deal with the problem that caused it in the first place, you're going to come back at some or the probability is you're going to come back.
Dr Rupy: I just want to underline that point because I don't think many people realise that 50%, so it's still 50% of presentations is either sudden death or presentation with a non-fatal heart attack.
Professor Kausik Ray: So if you think about, you know, the non-fatal part, how is that captured? Well, if you're somewhere and you're having a heart attack and there isn't an ambulance to take you to hospital and there isn't a unit to open up, well, you're killing off heart tissue while that artery is blocked. So, you know, there are there are other factors as well. So if you look at just so survival from heart attacks has improved. Part of that is better prevention, but part of it is we get people to hospital faster, you open up blood vessels faster, so you survive it. But if you look at rates of heart attacks, they haven't necessarily, you know, we might have seen a fall initially, but then we've seen other things coming in. So diabetes, obesity, for example. So there's always that, you know, is it, are you looking at just it happening, which is when the lining becomes unstable, or you're looking at deaths, because you might survive because I've just got a lot of ambulance and a lot of hospitals. But the number of heart attacks may not go down.
Dr Rupy: Because a lot of people use this sort of the prevalence of heart attacks and the fact that statins are so readily available over the last couple of years to say, well statins aren't having as much of an effect as they should be having. And I guess your answer to that would be, well it's not just about lipid control. There's all these other factors that we are not doing a great job of.
Professor Kausik Ray: Yeah, it it's, I mean, there was a guy that there's not a guy, there were a couple of people, um, that out of the states in the University of Liverpool and over decades of looking at trends, they'd estimated about half of the decline in heart attacks that we had seen or or improvement in survival, half of that were things like systems like, you know, heart attack centres, better ambulance, thrombolysis, clot busting agents, and the other 50% was risk factor control. So the point that you make about statins, so let me give you a salient point. So there's a a national registry in Sweden, small country, and essentially, you only actually leave the national register when you die or when you emigrate. So they've got really good data. So if you look at Sweden, the average age of a heart attack is about 63, 64, 62 to 64. Roughly 75% of people that came in with a heart attack, the day, the month, the year before weren't on a statin. So that means the day, the month, the year before, nobody thought this was going to happen, either the patient or healthcare. And so, you know, the concept about statins not preventing, well, 75% of the heart attacks, they weren't even on those. Then of the 25% that were on medications, for example, when you look at what they came in with, their cholesterol levels weren't too bad, but they had more in the way of risk factors, high prevalence of diabetes, they'd already had a prior heart attack, they were more likely to smoke. So the way of thinking about that is they've still progressed, they're progressors, they're frequent flyers if you will, despite everything that I'm doing. So that brings you back to genetic vulnerability and time.
Dr Rupy: Let's talk a little bit about cholesterol versus triglycerides because we've talked about the importance of cholesterol slightly, you know, it's a critical molecule, precursor to steroids, component of cell walls, produced endogenously.
Professor Kausik Ray: Yeah. So all cells produce cholesterol. This is this is why, you know, people sometimes say, well, can my blood cholesterol level get too low? Well, a newborn is born with a level of about 0.3 to 0.5 millimoles per litre. And when you get into adulthood, you know, 50% will range between about 2.3 and 3.8. So, but your cells will make it. You can get perfect hormone synthesis. If you're if you've got genetic variations that give you really low levels from birth, you get normal fertility, normal IQ, normal development and growth.
Dr Rupy: Yeah, because there's a lot that we can learn from genetic variants. So people who have naturally low levels of cholesterol throughout their whole life.
Professor Kausik Ray: Exactly. Yeah, yeah. Long time.
Dr Rupy: Yeah. So they they don't ever get atherosclerosis if I'm if I'm not.
Professor Kausik Ray: They have a lower risk of atherosclerosis. They they basically have normal health and function, they have a lower risk of cardiovascular disease basically, heart attacks and strokes.
Dr Rupy: But they have normal risk factors for things like cancer and diabetes and all the rest of it. It's just in the realm of CVD.
Professor Kausik Ray: It's the protection is against heart disease.
Dr Rupy: So that that is a big, you know, pointer for how critical lipid management is in the.
Professor Kausik Ray: Well, absolutely. And I and I hear, um, there are some people I've heard that talk about, well, there are 90 year olds that have high cholesterol, so cholesterol can't be that important. Well, the sick ones all died off. So the ones who get to 90, there's a survival bias. You know, they got to 90 despite that. But all of the others, that says nothing about cholesterol.
Dr Rupy: Yeah, yeah, yeah. So we can separate the anecdote of of folks who have got high cholesterol and have survived despite the high cholesterol because there's probably something and something else going on there. And so, so we have cholesterol. Triglycerides is the, yeah, so what what where is this created in?
Professor Kausik Ray: So so so basically, triglycerides are an energy source. So I mean, molecule for molecule, they will they will generate um more, so the unit of energy is ATP, they'll generate a lot more than say glucose will. And after a meal, your typically your levels will will go up. That gets packaged in the liver. The liver reproduces a particle that carries a little bit of triglyceride and some cholesterol, and that remodels and that that initial particle is something called VLDL, very low density lipoprotein. That just remodels in blood, it changes and it becomes the LDL particle. The triglyceride gets taken out, that gets stored in fat in fatty tissue and around your internal organs. And the worry about with triglycerides is is twofold. If it's really very high, so 10 millimoles per litre, we worry about a condition called pancreatitis. And, you know, that's a medical emergency, really painful, uncomfortable, and you you essentially have to look at those people in a in a completely different light. And so for example, a lot of those people, they can't handle carbohydrates and saturated and not not saturated fat, but fat and carbohydrates, largely because they have got metabolic disturbances that mean that they can't handle those types of compounds. So blood levels go, they lack the enzymes. More typically, triglycerides will be higher in people who are overweight or who are diabetic and the diabetes is poorly controlled, or who have a high alcohol intake. And so in that regard, you've got to take away the cause. So a lot of those people, for example, you want to treat the underlying source. So if you lost weight, you would improve insulin sensitivity. If that happened, the liver doesn't produce those initial particles that contain triglycerides. So you you basically have that benefit. Now, much lower levels, because there's lots of different particles that contain triglycerides. There's these really whopping great fluffy particles that we call chylomicrons after a meal. They're too big to get into the arterial wall. They get taken up by the liver. But those initial particles that we talked about, the VLDL particles, they are again, we think about them a little bit like we think about lipoprotein A as being molecule for molecule, a little bit nastier. So possibly twice as much. The the issue that we've got is is that imagine you go and you get a blood test done, that's a that's a Polaroid, that's a snapshot at a point in time. What's happening is it's it's a movie, it's a video. And particles are evolving. So when we look when you look up at the night sky, you see a lot of stars. You don't know if some of the ones have been born a million years ago or 10 million years ago. So the triglyceride containing particles are the recent ones, 1 million years ago. They sit around in blood, they've got a half life, plasma residence time we call this, about six hours. But the LDL particle, they sit around for about three to five days. So they're like been sitting around, those are your 10 million year old stars. So that's why it's really much, much more complex.
Dr Rupy: And so that's an interesting insight because I don't think I've ever thought about that from a perspective of a GP. We always ask our patients to fast for 12 hours before having a standard lipid panel. But if they've been eating fatty food during that week, does it stand to reason that their LDLC would be raised?
Professor Kausik Ray: So so I think that's a really good question. And I'll I'll give you a slightly laboured explanation. So the the real reason for the fasting is the so maybe we should start with just explaining a lipid panel. Um, so in the old days, all we were able to do is measure the total cholesterol. The problem is that's not very informative because there are all those different bits I was talking about. So you have to separate, uh, the you you precipitate out, you you you take out the HDL part, you measure the cholesterol cargo. And if you subtract that, then everything else is in those three bad particles that we can call non-HDL. So total cholesterol minus HDL cholesterol gives you non-HDL. But that's got three components. The vast majority of that will be the LDL particle. Even when lipoprotein A levels are really, really high in terms of concentration, there are fewer molecules because it's it's in the nanomole scale rather than millimole scale. So that's not going to give you a whopping great additive increase in your cholesterol level as such. But the triglycerides when they're high, so whatever the triglyceride is, if you divide by 2.2, that's roughly how much cholesterol that carries. So if it's 10, divide by 2.2 roughly, it's five units almost there of cholesterol next to the LDL. So, so in that scenario, we used to use something called the Friedewald formula. And we use this estimate of if the triglycerides are below about 4.5, divide by 2.2, calculate the cholesterol in the VLDL, and the LDL that you'd report was never measured, it was a calculated level. So now what's happened is most laboratories have moved to a different formula. And that's called the the Samson equation. And so that means that you can go all the way up to very low LDL cholesterol levels and accurately predict it, and you don't then get errors, and you could go up to a triglyceride level of about 9.4, 9.6. So now it's just the formula's changed. And you know, it's been validated multiple times with more expensive direct measurements that hospitals can't really run. So we know that that calculation is very reasonable. So that means it's great for our patients because you don't have to worry about the fasting state. And the beauty about a non-fasting measurement is it's a physiological pressure test. Because you also want to know when that person goes away, so one of my friends has got this thing's called called the Tex-Mex diet. And so basically in Texas, on a Friday, you will go, if you particularly got that tendency, genetic tendency towards this, you know, they're fine most of the time. But once they're having a Mexican meal with all of its goodies and a beer, that's when their triglycerides are going to go sky high. And that's when, you know, a lot of these people might be at risk of things like pancreatitis. But you know, joking aside, that's that's really helpful. And I know we like to maybe simplify things, but if you know what you're looking at, that full lipid profile, how you manage somebody that's got a high triglyceride who is at risk of a couple of things, there are different triggers, different drivers. You're going to ask about their alcohol intake. Is there a family history of pancreatitis? Are you overweight? And is that, you know, is your haemoglobin A1c, are you pre-diabetic? You're looking at all of those things and then you treat that. And then the triglycerides will go down with that. Um, but then on the other hand, if you've then got, you know, a high LDL and all the other things are are okay, that's your primary focus then. So that's why the full lipid panel really helps us.
Dr Rupy: Um, why don't we do direct measurement? Why do we use equations in the first place?
Professor Kausik Ray: Yeah, partly it's just cost. It's labour and time. Uh, and and I think that that was largely why we were using the Friedewald formula. And um, and that's why you had the whole fasting thing. Then about 11 years or so ago, many places said, let's just use non-HDL because most of non-HDL is LDL. The problem is that when we had add-on therapies, they were all using trials using LDL cholesterol. So the recommendations would be newer treatments, you know, that that would have would cost a little bit more. So you have to basically set the bar high, um, if you're a state's paying for it. And but that would be on the base of of an LDL above a certain level. So now imagine a whole country, everybody's just measuring non-HDL, and everybody goes, well, I've got no idea what the LDL is. So now it's actually coming back. And it has been for a little while. Because of the fact that essentially those treatments in terms of how the state pays for it, won't be on the base of the non-HDL, it'll be on the base of the LDL. So actually, it's a good thing. And now with the Samson formula, you don't need the direct.
Dr Rupy: And so, what are the other blood markers that if you were, I don't know, the czar of lipidology in the UK, that you would add to the standard lipid panel? Or do you think this gives us enough, uh, in the majority of cases, enough information about someone's, uh, risk profile as it pertains to lipids?
Professor Kausik Ray: So I think at the moment, if we basically made sure that all the laboratories had the Samson formula, I think some still don't. Um, but but I think in London, the vast majority do. And it's just programming in into the pathology system computer and getting them to do that and that's fine. I think LPA needs to be around in the entire country. You don't need to keep measuring it, you just need to measure it once and it's either normal or not. And so I think that's the key thing. We are always, you know, you are going to find different things that increase your risk. So, so for example, I probably should have said, it wasn't on my radar initially. So for example, heart disease risk is higher in people with chronic kidney disease. So you often don't know that unless you've measured something called EGFR. And so that's useful. You know, I mean, at 40, you wouldn't expect that. Let's say everything else is okay, but at 60, you have some infections or viral illnesses that damages your kidney or or something else. Now your risk has gone up. So it's not the same as it was in your 40s. And the other, the other thing I think now, you know, I'll I'll still see this with with patients is that haemoglobin A1c is not always kind of measured and and people still, you know, there's a lot of use of for diet and lifestyle, the glucose monitors that you see. They say, oh yeah, but I was using that and it was okay. But that's only one point in time. Haemoglobin A1c is the last three months. And it's an average of your good days and your bad days rather than, you know, the one that you're picking. I think there is another one that will come out, which is you talked a little bit about inflammation. So inflammation by, so there there are two things. One is if you get cholesterol into the blood vessel wall, your body responds, inflammation is body's way of trying to heal. So it responds by being more inflamed and trying to deal with that. But you could also have an inflammatory condition, rheumatoid patients with rheumatoid arthritis, HIV will have a slightly higher risk of cardiovascular disease than those without, for example. And there could be a direct effect of damaging the the lining of the wall that that accelerates that process. And then you've got the inflammatory response in the vessel wall itself. So a few years ago, I mean, we knew something called high CRP, you know, we can see down a microscope, lots of white cells in around cholesterol plaques, whether it's your neck, down your legs, in the blood vessels of your heart. And so people, you know, have talked about this and and been interested in this. And we've not had any direct ways of really targeting this. And the a few years ago, there was a trial done with with a compound that was targeting, there's a set of proteins that are called cytokines and they drive inflammation. So we know, we sometimes use this measure called CRP. That's not a cause, it's a downstream measure of lots of things. So if you're overweight, your CRP is going to be high. If you've got a low HDL, a high triglyceride, high glucose, you smoke, your CRP is going to be high. So what it does is in the body, there's like a master sensor, and it's called the NLRP3 inflammasome, and it's detecting lots of stresses in the body. And it responds by producing a set of proteins called cytokines, interleukin 1 beta, interleukin 6, and these cause inflammation, main drivers. We showed basically, or colleagues showed that targeting inflammation by targeting IL-1 beta reduced cardiovascular events by about 15%. So no more or less than we'd seen with other approaches, but it was on top of everything we were doing. And so that suggests that inflammation is causal. The problem with dampening down on inflammation is you kind of need inflammation to fight infections and other things. Your infection rates went up. And it was an expensive treatment as well.
Dr Rupy: What kind of treatment were we talking about?
Professor Kausik Ray: So it's a monoclonal. So it's something that we give autoimmune patients.
Dr Rupy: And so it sits around, but now we know autoimmune patients when we suppress the immune system, we're targeting other things like TNF alpha, etc. We know some of them might be more prone to infections as well. So that's the downside of that. Below interleukin 1 beta is interleukin 6, and that's currently being tested in a clinical trial at the moment where, you know, you take people who are inflamed, a high CRP, history of cardiovascular disease and renal disease because it seems to be the risk seems to be higher. And seeing actually whether giving these people this anti-inflammatory approach reduces their risk of heart attacks and strokes. It's also being looked at in people with heart failure because inflammation is part of so many different processes. And if you like, you know, is your normal response exaggerated like in people with rheumatoid arthritis, for example, you can see it can damage the joint. So if you can suppress that but in a highly targeted way, is that beneficial? So that may be something that we can add on in those individuals. And the other thing is, for example, weight loss, the biggest producer of interleukin 6 is adipose tissue. And so if you lose weight, CRP goes down, inflammatory markers go down. And that might be how some of the drugs, the GLP-1 agonists give cardiovascular benefit because they will give you some blood pressure reduction, a little bit of improvement in lipids, but there may be some direct effects on inflammation itself as well.
Dr Rupy: So the the markers that might be coming to market soon.
Professor Kausik Ray: CRP would be the one.
Dr Rupy: Okay, so so HSCRP.
Professor Kausik Ray: HSCRP rather than the right because essentially it's really very small. So if you have a a cough, a cold, a flu, your CRP will go high. And we're talking about levels here, you know, just above two milligrams per litre. So two, three, four that will give you a higher risk.
Dr Rupy: Yeah, yeah. And are there any others that are more sensitive or skewed more towards the risk profile for cardiovascular?
Professor Kausik Ray: Well, the the ideal would probably have been interleukin 6, but the problem is with that is it's going to be really quite, a, expensive. You've got to handle the sample in a particular way. So if you basically, you know, take a blood sample and you stick it on a shelf, it'll degrade. So you kind of need minus 80 and handling very, very carefully. Um, because you'll get natural degradation. So we use it for research and you know, we can write nice papers with it and you know, we get more information. But routine clinical use, we're not there yet. But then in terms of other markers, I mean, so one of the biggest revolutions was NT-proBNP for heart failure. You know, so basically, just lots and lots of work that was done with that in, so when your heart muscle gets stretched, when it's dilated, when it's failing, in that situation, NT-proBNP levels go up, the heart is trying to release a a protein that is essentially helping you wee out fluid so you don't overload. So levels of that, we know are useful for heart failure, breathlessness. When you come in with a heart attack, how do we distinguish between somebody with a non-cardiac issue from a heart attack? We can detect tiny amounts of heart muscle damage with something called troponin T or I. And so, but those in routine screening, let's say, probably we wouldn't be using. We use NT-proBNP for heart failure, breathlessness. Troponin probably not. So I think really the the one that will that we'll see more of, particularly if we have a treatment for those people who are inflamed, if you will, will be HSCRP.
Dr Rupy: With with regards to the anti-inflammation trials, so one's using monoclonal antibodies to dampen inflammation. Are there any trials looking at either nutraceuticals or things like omega-3, high dose omega-3 to reduce inflammation?
Professor Kausik Ray: So that's a good point. Um, okay, so we have got, so omega-3s came out largely as triglyceride lowering drugs. And years ago, we had a lot of trials that were kind of pre-statins. And there was a famous study called GISSI-Prevenzione that showed survival benefits, but very few people were on conventional treatment. So then when those studies were reproduced, we found basically that we didn't see the same benefit when background treatment and modern standard of care had changed. So then the question is, well, is there any benefit in that? But we'd we'd seen typically with higher doses of fish oils, omega-3s, there are two types. There's there's um EPA and DHA. EPA comes from fish. DHA comes from seeds, linoleic acid essentially. A lot of the stuff that you see over the counter, the dosage is really low, probably does no harm, but what we've done is multiple sets of trials. So the first thing is that the conventional combinations of DHA and EPA that we have available don't give you any added benefit in terms of heart attacks and stroke prevention. The second thing is when we've looked at absolutely pure EPA, so we did a trial called STRENGTH where we reduced triglycerides, reduced apoB, reduced CRP, reduced LDL a little bit, reduced triglycerides a lot, not a sign, not a sign of benefit. So how long was that trial? So three and a half years, about 13,000 people. We didn't see a benefit for that. Doesn't mean that lowering triglycerides is not good for pancreatitis, but it meant that, okay, that didn't show a benefit. But at the same time, there were colleagues that did a trial called REDUCE-IT using a different formulation. And that was four grams of a really ultra purified fish oil called icosapent ethyl. And they looked at people with high triglycerides and a low levels of HDL, already well managed otherwise. And they found a 25% reduction in heart attacks and strokes. The amount of benefit that they got was disproportionate to the changes in triglycerides. So that means that there must be something else that that's giving you that benefit. And with further work, what people have done now is essentially they've looked at how different types of fish oils, where they sit in the cell membrane. So cell membranes have a natural, it's a it's a bilayer if you will. So they're kind of look like tadpoles facing each other but a number of these. And this seems to sit at certain particular points within the bilayer whereas other compounds don't. And within that whole process, there's a natural process for resolving inflammation, and those are called resolvins. And if you basically enhance icosapent ethyl and EPA, you probably enhance the natural inhibitors of inflammation in the vessel wall. So what everybody's interested is is how, what determines the benefit if it's not the triglycerides. And you know, we know we've had at least three studies where we've seen that the drug itself, even with a slightly lower level, still gives a benefit. So it matters what you give and the amount you give. So we're basically starting, we've just had the first site visit of one of the sites. Hypothesis is you take people who have got inflammation in the vessel wall as measured by something called the fat attenuation index. And that that's basically like looking down a microscope with a times 100 lens. If you use a CT scan, a standard angiogram is like a times 10, you've got to have a lot of disease before you'll see anything. If you look at the walls with a calcium score, that's like a times 50 lens. Um, but this is actually giving you another level of granularity. And the hypothesis is if you take people with high triglycerides and they've got inflammation in the vessel wall, and I give half the people this compound, which is available, versus usual care, do I attenuate, do I dampen down on that inflammation? Because if that is the case, then we answer that question, and then we can go on and do a bigger, more definitive study. So we're just starting that.
Dr Rupy: Do you take fish oils?
Professor Kausik Ray: No, but I do take a lot of fish. My triglycerides are not elevated.
Dr Rupy: I've been taking statins for over 10 years.
Professor Kausik Ray: And that has an anti-inflammatory effect as well, right?
Dr Rupy: Yeah, it does. So it does have, we've got to be a little bit careful with that. So, so we know, for example, in test tubes, it will do it, it will it will reduce inflammation. What people typically think about reducing inflammation is looking at C-reactive protein and lowering that. Statins and this drug, bempedoic acid, they reduce, the liver makes CRP, and the statins themselves actually reduce the production. So something could reduce CRP and reduce the marker but not work upstream and reduce inflammation. It probably does have a slight anti-inflammatory effect, but nowhere near the amount of the treatments that are being tested.